The Only Medical Specialty That Survives on Lies
By Peter C. Gøtzsche | Brownstone Institute | September 8, 2025
I am a specialist in internal medicine and have a keen interest in statistics and research methodology.1 My general approach to science has led to publications in many different areas because people came to me when they suspected something fishy in their specialty.1
In 2007, midwife Margrethe Nielsen from the Danish Consumer Council wanted to find out if history was repeating itself. I offered her a PhD student scholarship and we found out that the withdrawal symptoms are very similar for depression drugs and benzodiazepines, but they were described as dependence only for the latter.2
This started my interest in psychiatry and I quickly realised that a lot else was also misrepresented in this specialty. The lies psychiatrists convey to the public are so common and so harmful for their patients that I published my own textbook of psychiatry where I document what is wrong in the official textbooks used by medical students and psychiatrists in training.3 Much of what is claimed in the textbooks is scientifically dishonest, and frequently cited research is often totally unreliable because the data were tortured till they confessed.4
Psychiatry is the only specialty I know of that causes more harm than good; in fact, vastly more harm than good.5 This disaster can only survive because psychiatrists constantly lie to the public about what they can achieve with their drugs. Psychiatrists also routinely violate elementary human rights about informed consent and use forced treatment even though it is harmful.5,6
The title of my most recent psychiatry book summarises the issues: “Is psychiatry a crime against humanity?”5 As you shall see, I am not exaggerating.
In January 2014, I published the article, “Psychiatry gone astray,” in a major Danish newspaper, which also came out in English.7 I described ten myths in psychiatry that are harmful for the patients:
Myth 1: Your disease is caused by a chemical imbalance in the brain.
Myth 2: It’s no problem to stop treatment with antidepressants.
Myth 3: Psychotropic drugs for mental illness are like insulin for diabetes.
Myth 4: Psychotropic drugs reduce the number of chronically ill patients.
Myth 5: Happy pills do not cause suicide in children and adolescents.
Myth 6: Happy pills have no side effects.
Myth 7: Happy pills are not addictive.
Myth 8: The prevalence of depression has increased a lot.
Myth 9: The main problem is not overtreatment, but undertreatment.
Myth 10: Antipsychotics prevent brain damage.
I explained why “Our citizens would be far better off if we removed all the psychotropic drugs from the market, as doctors are unable to handle them. It is inescapable that their availability creates more harm than good. Psychiatrists should therefore do everything they can to treat as little as possible, in as short a time as possible, or not at all, with psychotropic drugs.”
I hit some sore toes. There was an outcry, spearheaded by the drug industry and their paid allies among doctors and the media, but also the biggest debate in Denmark ever about psychiatric drugs.1,6 For more than a month, there wasn’t a single day without discussion of these issues on radio, TV, in newspapers, and at psychiatric departments. But sadly, the harmful business continued as usual.
The Facts
Psychiatric drugs do not have any specific effects, directed against a specific disease.8 Psychiatric disorders are merely a constellation of symptoms and psychiatric drugs have mainly two effects: They either sedate and numb people, or they stimulate them.
Brain-active drugs have such effects, e.g., also alcohol, opioids, cannabis, other psychedelics, and cocaine, but we don’t call such drugs antidepressants or antipsychotics. And the effect of antidepressants and antipsychotics is far below the minimally relevant effect, as established by the psychiatrists themselves in their research.3,6 It is therefore reasonable to say that they don’t work.
The most important effects of psychiatric drugs are not what you hear about. Because of the colossal overuse of the drugs, they are the major reason that our prescription drugs are the leading cause of death, ahead of heart disease and cancer.9 One in five citizens is on an antidepressant, which can cause falls, and when elderly people break their hip, one-fifth will die within the next year.
Many of those who don’t die will fare badly anyhow. In all countries where the relationship has been examined, the rates of disability pensions go up in tandem with increased usage of psychiatric drugs.10
You don’t hear much about sexual disturbances either. The so-called happy pills harm the sex life in half the patients, and in half of those patients, the harm is unacceptable.11 In some patients, the harms are irreversible and continue after the patients come off their drugs, which has led to suicide.12
The Lies
Psychiatrists, particularly those in high positions, routinely lie to the public with the intent to protect their guild interests and their financial interests, which are huge. In the US, there are more psychiatrists collecting payments from the pharma industry than any other type of specialist.13
The American Psychiatric Association (AMA) is corrupt. Many of the psychiatrists who invented the most foolish diagnoses in its Diagnostic and Statistical Manual (DSM) for psychiatric disorders, which expanded hugely the market for psychiatric drugs, were on industry payroll. But they are not open about it. The DSM-5-TR panel members received $14 million in undisclosed industry funding.14 To a European, this is an obscene level of corruption.
The worst lie is this one: Psychiatrists routinely tell their patients that they are ill because they have a chemical imbalance in the brain and that they will receive a drug that fixes this.
An associated lie is that withdrawal effects, when the patients try to come off their drugs, are trivial, and not withdrawal effects at all, but signs that their disease has relapsed and that they still need the drugs.15
In 2018, leaders in the UK Royal College of Psychiatrists wrote in the Times that, “in the vast majority of patients, any unpleasant symptoms experienced on discontinuing antidepressants have resolved within two weeks of stopping treatment.”5 A group of clinicians and academics, including me, wrote to the authors that their statement was incorrect and that the College’s own survey of over 800 patients had found that withdrawal symptoms were experienced by 63% of the patients and that a quarter reported anxiety lasting more than 12 weeks.
The College immediately removed its survey from its website and when they refused to correct the error, we made our complaint public, which was covered by the BBC. Later, psychiatrist Sir Simon Wessely, previous president of the College, rejected any link between the pills and suicide and stated categorically in a podcast that they are “not addictive.”
We then published a most damning letter in the BMJ.16 Since guidelines from the National Institute for Health and Care Excellence (NICE) stated that withdrawal symptoms were “usually mild and self-limiting over about 1 week,” we asked for the evidence. NICE provided two short review articles, neither of which supported the one-week claim, and both articles cited numerous sources that contradicted it!
The embarrassment was now so big that the College needed to change its stance and NICE updated its guidelines.
This is one of the very rare instances where protests about psychiatry’s lies have led to any change. But the organised denial just continued. In 2025, a highly flawed systematic review in JAMA Psychiatry claimed that antidepressant withdrawal is not a problem.17,18 As usual, the authors postulated that depression after discontinuation is indicative of depression relapse.
To spread a little candlelight in the psychiatric darkness, I invented the term abstinence depression, which is not a true depression.3,18 The fact is that about half of the patients experience withdrawal effects; in half of the cases they are severe; and when patients try to stop, they often become worse than they were before they started on the drug.19 Moreover, the longer one is on the drugs, the higher the risk of withdrawal.19,20
The lies about a chemical imbalance and that abstinence symptoms are signs of relapse keep patients on their drugs for many years. Why would they ever stop when it is so clear that they need the drugs? But we don’t argue this way in relation to abuse of alcohol or narcotics. The patients never had a chemical imbalance causing their problems; but the drugs created one21,22 and caused harm.
Another big selling point is that you only need to treat a couple of patients to benefit one of them. This is also a huge lie. Psychiatric drugs cannot cure anyone. And the illusion of huge benefits is obtained by statistical manipulation.23 The trick is to dichotomise disappointing outcome data on a ranking scale and talk about response rates instead.24
This statistical hocus-pocus can convert a non-existing benefit into an almost doubling of the response rate,24 which looks very impressive. But as psychiatrist Joanna Moncrieff wrote, it is spinning straw into gold transforming ineffectiveness into the much-trumpeted idea that antidepressants work.25
The number needed to treat to benefit one patient (NNT) doesn’t exist because more patients are harmed than those who benefit. There can therefore only be a number needed to harm (NNH), which is two for sexual harms caused by antidepressants.11
Harms and benefits are rarely measured on the same scale, but when patients in a placebo-controlled trial decide whether it is worthwhile to continue in the trial, they make a judgment about if the benefits they perceive exceed the harms. My research group found that 12% more patients dropped out on a depression pill than on placebo (P < 0.00001).26 Thus, the patients will benefit by NOT being treated with antidepressants. They prefer a placebo.
More Examples of Institutional Betrayal
The US National Institute for Mental Health (NIMH) is the most prestigious psychiatric institution in the world. In 2022, Thomas Insel, its director from 2002 to 2015, called “America’s psychiatrist,” published the book, “Healing: Our Path From Mental Illness to Mental Health.”
Insel takes on the role of a drug rep, selling the wonders of psychiatric drugs to the public, but his book is misleading and dishonest.5 It starts already with the title. Psychiatric drugs cannot heal mental disorders, and the path the psychiatrists have taken is not from mental illness to mental health, but from bad to worse. Clearly, Insel makes an unintended case for abolishing psychiatry even though he tries to support it.27
The book reflects the thinking of psychiatric leaders everywhere and encapsulates how psychiatry has consistently betrayed public trust and misinformed the public, and that it will never tell the public the truth about psychiatric drugs.
Being a former NIMH director, Insel had an ethical obligation to tell his readers about the negative long-term outcomes of treatment with psychiatric drugs, as documented in expensive and prestigious research funded by the NIMH, e.g. the STAR*D trial in depression – a $35 million fraud – the MTA trial in ADHD, and the CATIE trial in schizophrenia.5 He didn’t, even though the NIMH is the only institution in the world that funds the big, long-term drug trials. As psychiatric leaders always do, Insel sacrificed the patients and protected the psychiatric guild by keeping the long-term studies financed by his own institute hidden.
In January 2025, I notified the UK drug regulator, the Medicines & Healthcare products Regulatory Agency (MHRA), that the package inserts for antidepressants — called patient information leaflets (PIL) — contain false statements about depression being caused by a chemical imbalance, and I called for the misleading messages to be removed.28
The MHRA refused and when I sent a letter about this to four major UK newspapers and the Royal College of Psychiatrists with Joanna Moncrieff and others, they didn’t even have the courtesy to respond.
To paraphrase Lenin, editors of leading medical journals also behave like useful idiots for psychiatry and the drug industry. On 10 May 2025, an anonymous editorial in the Lancet, “50 years of SSRIs: weighing benefits and harms,” did little of what its title promised. It praised the drugs based on flawed research and glossed over the harms. When I pointed out how misleading the editorial was in a letter to the editor, it was rejected.28
Many Cochrane reviews of psychiatric drugs also contain misleading praises of the drugs and are garbage in, garbage out exercises that uncritically reproduce the flawed data the drug industry has published.1,5,29-31
The Lie That Drugs Can Prevent Suicide
Despite their pompous designation, “State of the Art” articles in leading medical journals are usually misleading and they are particularly dishonest in relation to suicides.1 A 19-page review in the BMJ claimed that depression drugs, lithium, antiepileptics, clozapine, ketamine, and electroshock can decrease the risk of suicide.32 None of the 159 references were convincing;33 the package inserts for depression drugs warn against the risk of suicide; and the package inserts for antiepileptics state that they double the risk of suicide!
In a 14-page Lancet suicide seminar from 2022, the authors tried to resurrect the lie about the chemical imbalance but the two articles they cited were gobbledygook.34,35 Among risk factors for suicide, they mentioned substance use but not depression pills, antiepileptics, or the psychiatric profession itself.35,36 A Danish register study of 2,429 suicides showed a very marked dose-response relationship:36 The closer the contact with psychiatric staff, the greater the risk of suicide.
Compared to people who had not received any psychiatric treatment in the preceding year, the adjusted rate ratio for suicide was 44 for people who had been admitted to a psychiatric hospital.36 Such patients would of course be expected to be at greatest risk of suicide because they were more ill than the others (confounding by indication), but the findings were robust and most of the potential biases in the study were actually conservative, i.e. favoured the null hypothesis of there being no relationship. An accompanying editorial noted that there is little doubt that suicide is related to both stigma and trauma and that it is entirely plausible that the stigma and trauma inherent in psychiatric treatment—particularly if involuntary— might cause suicide.37
The Lancet authors wrote that there is a possibility of exacerbating suicidal thoughts. Wrong. It is not a possibility; it is a fact. None of the 142 references were to any of the many meta-analyses showing that depression pills increase the suicide risk compared to placebo. The authors even claimed, with no references, that drug treatment can reduce the suicide risk. Which miraculous drugs can do this?
They also noted that some research has found an association with increased risk of suicide-related outcomes in young people. This is also dishonest. When the FDA looked at all the randomised trials, they found a causal relation and not just an association.
In 2023, the “experts” failed us badly again. A 16-page article in BMJ about suicide in young people, with 169 references, mentioned some risk factors, e.g. living in a home with firearms, but not depression drugs, which they recommended with “increased monitoring by the prescribing physician.”38 This is a fake fix, as people may kill themselves suddenly and unexpectedly.39
The authors considered a risk difference of 0.7% for suicidal ideation or suicide attempt between drug and placebo small and even dismissed it: “Data from more recent pediatric antidepressant trials have not shown differences between drug and placebo.” The review they quoted cannot be used to such effect and for rare events, it is unacceptable to lose statistical power by including only “recent” trials. Moreover, the review only included published trial reports, which we know have omitted many suicide attempts and suicides, even in children.6,39 It is irresponsible of the BMJ to publish such dangerous nonsense.
In 2023, I called for retraction of three fraudulent trial reports that had omitted suicidal events in children.40 Even though my letter was co-signed by 10 people who each lost a child or spouse to suicide as a direct consequence of being prescribed an antidepressant drug for a non-psychiatric condition, my request was turned down by both involved journals.41
Annette Flanagin, Executive Managing Editor, Vice President, Editorial Operations JAMA and JAMA Network, replied: “We shared your letter with the author of the study published in Archives of General Psychiatry and he does not identify any new concerns. Similarly, we do not find new evidence in support of your request to retract this article.”
So, JAMA and Graham Emslie, who omitted two suicide attempts on fluoxetine, do not think this is something to bother about. When I contacted the journal’s owner, Elsevier, they did not engage with our concerns but directed me back to the journal.
Douglas K. Novins, Editor-in-Chief, Journal of the American Academy of Child & Adolescent Psychiatry (JCAAP), wrote to me that, “Following guidelines developed by the Committee on Publication Ethics (COPE),” they had thoroughly reviewed my “critique, as well as the responses provided by the papers’ authors. We are satisfied that the critiques of the papers as outlined do not merit retraction.”
It is hard to see how Novins could have followed the COPE guidelines, as the two trial reports, by Emslie and Martin Keller, are clearly fraudulent.
In 2023, I did a Google search on suicide and antidepressants, which confirmed that the public is being massively and systematically misinformed.42,43 One of the top 10 posts was from the Danish Centre for Suicide Research that reported that depression drugs increase the risk of repeated suicide attempts by 50%.44 The research was supported by Lundbeck, and after the researchers had adjusted their analyses for many factors including psychiatric contact and use of various psychiatric drugs, they concluded that the pills do not increase the risk of suicide. It is plain wrong to adjust for something that is part of the causal chain, as it may remove a true association, but the authors surely pleased their funder.
Another post was a comment I made on the Danish Board of Health’s website.45 Poul Videbech, a national icon in depression, had claimed in the Board’s journal, Rational Pharmacotherapy, that undertreatment with depression drugs is dangerous because of the suicide risk. This cannot be correct because the drugs increase the risk of suicide.
When I searched the Internet to find out what the “experts” opine currently, I found a systematic review in the psychiatrists’ flagship journal, American Journal of Psychiatry.46 It was about “evidence-based strategies,” but already the abstract was blatantly false. It claimed that “Meta-analyses find that antidepressants prevent suicide attempts.”
I don’t know of any other medical specialty whose practitioners lie systematically to the public in matters of life and death and claim the opposite of what is true.
In June 2025, I gave a talk in Capitol about suicides caused by antidepressants, invited by US war veterans who are routinely given these drugs for their war traumas.47 As expected, the effect of the veterans’ suicide prevention programme has been a notable increase in suicides corresponding to a similar increase in antidepressant usage.48,49
In the surreal upside-down world of psychiatry, all suicide prevention initiatives I have come across have included drugs that increase suicides!50
There was a press conference outside the Capitol,47 but the media are not keen to write stories about antidepressants killing people. I only saw an article in the Wall Street Journal, which I tweeted about:
Combat cocktails: US war veterans are destroyed and kill themselves because of psychiatric polypharmacy. Wall Street Journal https://bit.ly/4fjkz5P.
Antidepressants Harm the Unborn Child
New winds are blowing in the US, which could profoundly change healthcare for the better.51 On 21 July 2025, the FDA held a two-hour seminar about the possible harms to the foetus of treating pregnant women with antidepressants.52 For the first time, this crucial issue was honestly debated at the FDA, by good scientists, but this could not be tolerated by the professional liars.
There was a howl of outrage from psychiatric organisations and mainstream media that accused the FDA’s panel of being alarmingly unbalanced and of spreading misinformation,53-55 which was not at all the case.
The American Psychiatric Association (AMA) wrote to the FDA four days after the meeting that it was “alarmed and concerned by the misinterpretations and unbalanced viewpoints shared by several of the panelists… This propagation of biased interpretations at a time when suicide is a leading cause of maternal death within the first postpartum year could seriously hinder maternal mental health care. The inaccurate interpretation of data, and the use of opinion, rather than the years of research on antidepressant medications, will exacerbate stigma and deter pregnant individuals from seeking necessary care.”
The AMA could hardly have been more dishonest. Antidepressants double not only the risk of suicide but even actual suicides.49,56
Without mentioning the pregnancy issue, the AMA circled the wagons again, in a tweet on 28 August:57
“IMPORTANT: Decades of rigorous research, randomized clinical trials, peer-reviewed studies, meta-analyses, national registry studies, and FDA oversight show that psychiatric medications are safe and effective. Medications like SSRIs can be lifesaving if they are taken as directed under the care of an appropriately licensed healthcare professional. Learn more: https://ow.ly/RWEQ50WNJeI.“
In just two sentences, the AMA propagated three lies. No psychiatric drug is safe. They all kill people, to a substantial degree.1,3,5,6,9 And it has never been documented that SSRIs can be life-saving while it has been documented that they take many lives. They cause suicides and homicides6 and lead to falls in the elderly,9 and when they break their hip, one-fifth will die within the next year. Psychiatric medications are not effective either, e.g. the effect of antidepressants and antipsychotics is far below the minimally relevant effect, as established by the psychiatrists themselves in their research.5,6
Not even when there is clear evidence, both from studies in animals and humans,52-55 that our children are being harmed by psychiatric drugs before they are even born, do we see any admission from the AMA that it is wrong to treat pregnant women with antidepressants. They prefer to continue lying.
Antidepressants should be banned for use in pregnant women. Psychotherapy is more effective, as it has enduring effects,5,6 and it won’t harm the unborn child.
Reactions to AMA’s Tweet
Increasingly, the public is waking up to psychiatry’s deceptions. People are not so dumb as the AMA thinks they are, which the retweets to AMA’s tweet57 demonstrate:
“The FDA issues a black box warning for all SSRI’s indicating increased risk of suicidal thoughts and behaviors, particularly in children, adolescents, and adults under 25. How could the American Psychiatric Association make such a claim? (sic) Isn’t doing so extremely unethical?!”
“The APA is lying to you. SSRIs are neither safe nor effective. NOT EVEN CLOSE. And they do not magically perform better under the care of a licensed professional. Them’s the facts.”
“Anytime I hear experts so-called say something is safe and effective. I immediately know that that is not the case. Thank you for confirming my suspicion.”
“Merriam-Webster defines ‘safe’ as ‘free from danger, harm, or risk.’ All classes of psych meds include black box warnings about serious or life-threatening adverse effects risks.”
“How safe is sudden death? Some of those meds can cause that.”
“Life-taking. My adult son didn’t make it past 6 weeks after his #PillPusher prescribed SSRIs within 15min of meeting him.”
“What percentage of patients who take SSRIs are cured and can stop taking them?”
“I don’t know a single person who has been cured by psychiatric drugs.”
“The good ‘ol APA, brought to you by Pfizer. Maybe they will make a med for cognitive dissonance soon?”
“Psychiatry is quackery. Read the book Anatomy of an Epidemic by Robert Whitaker!”
“Psychiatry is one of the dumbest religions.”
A retweeter showed this picture of Mr. Bean, which sort of explains it all:
Conclusions
Psychiatry is a totally corrupt specialty, ethically, scientifically, and financially, with devastating consequences for the patients, their relatives and friends, and for our national economies.
Psychiatry is a crime against humanity that must be stopped.5 It should not be a medical specialty, and patients with mental health issues should not be treated by medically trained doctors because the existing approaches, which focus on drugs, are not working.
In the UK, mental health disability has almost tripled in recent decades, and the gap in life expectancy between people with severe mental health issues and the general population has doubled.58 The World Health Organisation (WHO) and the United Nations have therefore recently called for systematic mental health reform emphasising psychosocial interventions.58
My advice to patients is: If you have a mental health issue, don’t see a psychiatrist. It is too dangerous and might turn out to be the biggest error you made in your entire life.12,59 Don’t look up a family doctor either, as they are also programmed to make psychiatric diagnoses and hand out psychiatric pills.
References
1 Gøtzsche PC. Whistleblower in healthcare (autobiography). Copenhagen: Institute for Scientific Freedom 2025; April 8 (freely available).
2 Nielsen M, Hansen EH, Gøtzsche PC. What is the difference between dependence and withdrawal reactions? A comparison of benzodiazepines and selective serotonin re-uptake inhibitors. Addiction 2012;107:900–8.
3 Gøtzsche PC. Critical Psychiatry Textbook: a new psychiatry is needed. Copenhagen: Institute for Scientific Freedom 2023; May 17.
4 Mills JL. Data torturing. N Engl J Med 1993;329:1196-9.
5 Gøtzsche PC. Is psychiatry a crime against humanity? Copenhagen: Institute for Scientific Freedom; 2024 (freely available).
6 Gøtzsche PC. Deadly pPsychiatry and Organised Denial. Copenhagen: People’s Press; 2015.
7 Gøtzsche PC. Psychiatry gone astray. Mad in America 2014; Jan 28.
8 Moncrieff J. The Myth of the Chemical Cure: A Critique of Psychiatric Drug Treatment. Basingstoke: Palgrave Macmillan; 2007.
9 Gøtzsche PC. Prescription Drugs Are the Leading Cause of Death. Brownstone Journal 2024; April 16.
10 Whitaker R. Anatomy of an Epidemic, 2nd edition. New York: Broadway Paperbacks; 2015.
11 Montejo A, Llorca G, Izquierdo J, et al. Incidence of sexual dysfunction associated with antidepressant agents: a prospective multicenter study of 1022 outpatients. Spanish Working Group for the study of psychotropic-related sexual dysfunction. J Clin Psychiatry 2001;62 (suppl 3):10–21.
12 Gøtzsche PC. Mental Health Survival Kit and Withdrawal from Psychiatric Drugs. Ann Arbor: L H Press; 2022.
13 Staton T. Psychiatrists dominate doc-payment database. Fierce Pharma 2010; Oct 25.
14 Burton KW. DSM-5-TR Panel Members Received $14M in Undisclosed Industry Funding. Medscape 2024; Jan 10.
15 Gøtzsche PC, Demasi M. Interventions to help patients withdraw from depression drugs: A systematic review. Int J Risk Saf Med 2024;35:103-16.
16 Davies J, Read J, Hengartner MP, et al. Clinical guidelines on antidepressant withdrawal urgently need updating. BMJ 2019;365:l2238.
17 Kalfas M, Tsapekos D, Butler M, et al. Incidence and nature of antidepressant discontinuation symptoms: a systematic review and meta-analysis. JAMA Psychiatry 2025;Jul 9:e251362.
18 Gøtzsche PC. Exposing the Lie That Antidepressant Withdrawal Symptoms are Mild and Short-Lived. Brownstone Journal 2025; July 25.
19 Davies J, Read J. A systematic review into the incidence, severity and duration of antidepressant withdrawal effects: Are guidelines evidence-based? Addict Behav 2019;97:111-21.
20 Horowitz MA, Buckman JEJ, Saunders R, et al. Antidepressants withdrawal effects and duration of use: a survey of patients enrolled in primary care psychotherapy services. Psychiatry Res 2025;350:116497.
21 Moncrieff J, Cohen D. Do antidepressants cure or create abnormal brain states? PLoS Med 2006;3:e240.
22 Moncrieff J, Cooper RE, Stockmann T, et al. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry 2023;28:3243-56.
23 Gøtzsche PC. Number needed to treat with a psychiatric drug to benefit one patient is an illusion. Mad in America 2022; Dec 13.
24 Gøtzsche PC. Response Rates in Psychiatric Drug trials are Statistical Nonsense. Brownstone Journal 2025; July 11.
25 Moncrieff J. Chemically Imbalanced: The Making and Unmaking of the Serotonin Myth. Padstow: Flint; 2025.
26 Sharma T, Guski LS, Freund N, et al. Drop-out rates in placebo-controlled trials of antidepressant drugs: A systematic review and meta-analysis based on clinical study reports. Int J Risk Saf Med 2019;30:217-32.
27 Whitaker R. Thomas Insel makes a case for abolishing psychiatry. Mad in America 2022; Apr 30.
28 Gøtzsche PC. Protecting the false narrative about antidepressants. Mad in America 2025; July 7.
29 Gøtzsche PC. Cochrane recommends antidepressants for anxiety in a garbage in, garbage out review. Mad in America 2025; July 29.
30 Gøtzsche PC. Garbage in, garbage out: the newest Cochrane meta-analysis of depression pills in children. Mad in America 2021; Aug 19.
31 Gøtzsche PC. Cochrane reviews of psychiatric drugs are untrustworthy. Mad in America 2023; Sept 14.
32 Bolton JM, Gunnell D, Turecki G. Suicide risk assessment and intervention in people with mental illness. BMJ 2015;351:h4978.
33 Gøtzsche PC. No psychiatric drugs have been convincingly shown to decrease suicides. BMJ 2015; Dec 10.
34 Knipe D, Padmanathan P, Newton-Howes G, et al. Suicide and self-harm. Lancet 2022;399:1903-16.
35 Gøtzsche PC. A hopelessly flawed seminar in “The Lancet” about suicide. Mad in America 2022; June 1.
36 Hjorthøj CR, Madsen T, Agerbo E, et al. Risk of suicide according to level of psychiatric treatment: a nationwide nested case-control study. Soc Psychiatry Psychiatr Epidemiol 2014;49:1357–65.
37 Large MM, Ryan CJ. Disturbing findings about the risk of suicide and psychiatric hospitals. Soc Psychiatry Psychiatr Epidemiol 2014;49:1353–5.
38 Hughes JL, Horowitz LM, Ackerman JP, et al. Suicide in young people: screening, risk assessment, and intervention. BMJ 2023;381:e070630.
39 Gøtzsche PC. Depression drugs have been shown to double the risk of suicide in young people and should not be used. BMJ 2023; April 26.
40 Gøtzsche PC. Call for retraction of three fraudulent trial reports of antidepressants in children and adolescents. Institute for Scientific Freedom 2023; Aug 3.
41 Gøtzsche PC. Medical journals refuse to retract fraudulent trial reports that omitted suicidal events in children. Mad in America 2024; Mar 18.
42 Gøtzsche PC. The lie that antidepressants protect against suicide is deadly. Mad in America 2023; Nov 28.
43 Gøtzsche PC. So-called suicide experts recommend antidepressants, which increase suicides. Mad in America 2024; Oct 24.
44 Jakobsen SG, Christiansen E. Selvmordsforsøg og antidepressiva. Center for Selvmordsforskning 2019; Dec.
45 Gøtzsche PC. Misinformation om antidepressiva og selvmord. http://www.irf.dk 2015; March 5.
46 Mann JJ, Michel CA, Auerbach RP. Improving suicide prevention through evidence-based strategies: a systematic review. Am J Psychiatry 2021;178:611-24.
47 Harris L. Veterans Take Their “War Cry For Change” to Capitol Hill. Mad in America 2025; June 14.
48 Gøtzsche PC. Suicides increase after national suicide prevention introduced. Mad in America 2025; Feb 20.
49 Gøtzsche PC. Observational studies confirm trial results that antidepressants double suicides. Mad in America 2025; Feb 8.
50 Gøtzsche PC. So-called suicide experts recommend antidepressants, which increase suicides. Mad in America 2024; Oct 24.
51 Kennedy: A new time for America? Filmed interview with Peter C. Gøtzsche. Broken Medical Science 2025; Jan 12.
52 FDA Expert Panel on Selective Serotonin Reuptake Inhibitors (SSRIs) and Pregnancy. YouTube 2025; July 21.
53 Whitaker R. Not even the unborn are safe from psychiatric harm. Mad in America 2025; Aug 23.
54 Moncrieff J, Urato A. Antidepressants in Pregnancy -Turning a Blind Eye, Again. Mad in America 2025; Aug 25.
55 Gøtzsche PC. Psychiatrists Deny the Harm of Antidepressants for the Fetus. Brownstone Journal 2025; Aug 30.
56 Hengartner MP, Plöderl M. Reply to the Letter to the Editor: “Newer-Generation Antidepressants and Suicide Risk: Thoughts on Hengartner and Plöderl’s ReAnalysis.” Psychother Psychosom 2019;88:373-4.
57 American Psychiatric Association tweet. X 2025; Aug 28.
58 Shifting the balance towards social interventions: a call for an overhaul of the mental health system. Beyond Pills All-Party Parliamentary Group 2024; May.
59 Breggin P. The most dangerous thing you will ever do. Mad in America 2020; March 2.
Dr. Peter Gøtzsche co-founded the Cochrane Collaboration, once considered the world’s preeminent independent medical research organization. In 2010 Gøtzsche was named Professor of Clinical Research Design and Analysis at the University of Copenhagen. Gøtzsche has published more than 97 over 100 papers in the “big five” medical journals (JAMA, Lancet, New England Journal of Medicine, British Medical Journal, and Annals of Internal Medicine). Gøtzsche has also authored books on medical issues including Deadly Medicines and Organized Crime.
Your Spouse Started Antidepressants and Became a Stranger
The hidden crisis and why it happens

By Dr. Roger McFillin | Radically Genuine | August 7, 2025
“I don’t know who this person is anymore,” James told me, his voice cracking as he described his wife of fifteen years. “She started Zoloft eight months ago for some mild anxiety about work. Now she’s rewritten our entire history together. According to her new narrative, I’ve been emotionally abusive for years. She’s filed for divorce, moved in with some guy she met at a yoga retreat, and told our kids that daddy was never really there for them.”
He paused, searching for words. “The strangest part? She seems completely unbothered by destroying our family. It’s like she’s watching it happen from outside her own body.”
Welcome to the SSRI marriage apocalypse: a phenomenon so widespread that entire online communities have formed to support its casualties. Spouses gathering in digital refugee camps, comparing notes about partners who transformed into unrecognizable strangers after starting antidepressants. The stories are eerily similar: personality changes, moral compass spinning wildly, empathy evaporating, sexual connection obliterated, and a strange, detached willingness to torch everything they once held sacred.
But here’s what makes my blood boil: The mental health establishment celebrates these relationship demolitions as therapeutic breakthroughs. “The medication lifted their mood enough to finally leave that toxic relationship!” they’ll proclaim, completely ignoring that the “toxicity” might be a drug-induced fabrication. This is my fundamental criticism of the therapy industry: therapists attach to their client’s inner world as if it’s absolute fact, unquestionable truth.
Even without SSRIs, people alter reality and create stories to cope with pain. But add psychiatric drugs to the mix, and you’ve got modern therapists providing unfettered validation to chemically distorted narratives, rarely approaching cases with empirical scrutiny. They jump right on the victim mindset, and in many cases, actively create it. “Yes, you were trapped in an abusive marriage!” they’ll affirm to someone whose brain chemistry has been so altered they couldn’t recognize genuine love if it slapped them in the face.
The Spell-Binding Effect
Dr. Peter Breggin, Harvard-trained psychiatrist and former consultant to the National Institute of Mental Health who’s spent decades exposing the dark underbelly of his own profession, called it “medication spellbinding”: the insidious way psychiatric drugs prevent users from recognizing their own drug-induced dysfunction. (I’m actually traveling to Dr. Breggin’s home next week to interview him, and you can bet your ass I’ll be drilling deep into this spell-binding phenomenon.) It’s not just that SSRIs change you; they rob you of the ability to perceive that you’ve been changed. You become a stranger to yourself while believing you’re finally seeing clearly.
“Lisa” sat across from me six months after stopping Lexapro, tears streaming down her face. “I feel like I’m waking up from a nightmare I created. I had an affair. I told my husband of twenty years that I’d never really loved him. I was prepared to walk away from my children without a second thought. Now I look back and think, ‘Who was that person?’ But at the time, it all made perfect sense. I felt nothing. No guilt, no remorse, no connection to my old life. It was like living in emotional Novocain.”
This is your brain on SSRIs: chemically castrated not just sexually but emotionally, morally, spiritually. The same serotonergic manipulation that’s supposed to lift your mood also severs the invisible threads connecting you to everything that matters. But you won’t realize it’s happening because the drug disables your ability to recognize its own effects.
The psychiatric establishment has convinced millions that flooding the brain with serotonin is as benign as taking vitamin C. They’ve never bothered to mention that serotonin doesn’t just regulate mood; it shapes moral reasoning, empathy, pair bonding, sexual response, and the entire constellation of neurochemical processes that make us capable of authentic human connection.
This is why I have profound concerns about prescribing these drugs during critical developmental periods. When you chemically alter serotonin in a developing adolescent brain, you’re not just tweaking mood; you’re potentially rewiring their capacity for intimacy, identity formation, and even sexual orientation. The explosion of gender dysphoria cases perfectly paralleling the mass prescribing of SSRIs to teenagers? That’s not a coincidence worth ignoring. That’s a red flag the size of Texas that nobody wants to acknowledge because it threatens both Big Pharma profits and progressive orthodoxy.
When “Treatment” Becomes Home-Wrecking
Here’s what the hundreds of stories flooding my inbox and online communities reveal: SSRIs create a spectrum of personality destruction, and we’re essentially playing Russian roulette with human consciousness. The response varies wildly because we’re experimenting with pharmaceutical compounds that fundamentally alter human nature itself.
For some, there’s an almost immediate activation syndrome (conveniently buried in the clinical trial data). Within days or weeks, they experience impulsivity that would make a teenager blush. Reckless spending, sexual promiscuity, acting without any consideration of consequences. One woman described it perfectly: “It was like someone disconnected the brake pedal in my brain. I was all accelerator, no caution.” Affairs happen in this state. Life-destroying decisions get made. Families implode while the person feels euphoric about the destruction.
For others, it’s the slow slide into emotional death. The detachment creeps in gradually: first, colors seem less vibrant. Music loses its emotional pull. Then comes the relationship anesthesia. “I just don’t feel anything for him anymore,” becomes the refrain, as if discussing a roommate rather than a life partner. The sexual dysfunction arrives not just as decreased libido but complete genital numbness, the physical capacity for intimate bonding chemically severed. But instead of recognizing this as drug-induced castration, it gets reframed: “I guess I was never really attracted to them.”
The empathy erosion is perhaps the most chilling. The person who once cried at commercials now watches their partner’s pain with scientific detachment. Children become logistical problems to solve. Love transforms into a word they remember but can’t feel. It’s not cruelty; it’s worse. It’s the presence of absence where humanity used to live.
The therapy industrial complex, thoroughly indoctrinated in the chemical imbalance mythology, validates every drug-distorted thought. Your couples therapist, who hasn’t bothered to research SSRIs beyond pharmaceutical marketing materials, encourages your drugged spouse to “trust their feelings” and “honor their truth,” never once considering that their feelings are chemically manufactured and their truth is pharmaceutical fiction.
Post SSRI Sexual Dysfunction (PSSD)
Post-SSRI Sexual Dysfunction (PSSD) is the dirty secret of psychiatry that could bring down the entire house of cards if people truly understood its implications. We’re not talking about temporary side effects here. We’re talking about permanent sexual castration that persists, even after stopping the drugs.
But PSSD isn’t just about sex. It’s about the complete severing of the embodied experience of human connection. The neurochemical pathways that create sexual arousal are the same ones involved in emotional bonding, passionate engagement with life, and the felt sense of love itself. When SSRIs nuke these systems, they don’t just steal orgasms; they steal the capacity for embodied intimacy altogether.
And now we have hard scientific evidence for what these communities have been screaming into the void. A 2019 study published in Translational Psychiatry by Rütgen and colleagues finally confirmed what Big Pharma has desperately tried to suppress: SSRIs don’t improve empathy in depression; they systematically destroy it.
The researchers found that after just three months of antidepressant treatment, patients showed significant decreases in both emotional empathy and brain activity in regions crucial for empathic responding. The more their depression “improved,” the less they could feel others’ pain. They literally measured the chemical assassination of human compassion.
But here’s what nobody wants to admit: the pharmaceutical industry measures “improvement” in depression by how much less you feel. Can’t cry at your mother’s funeral? Success! Don’t feel devastated when your child is hurting? Treatment is working! Unable to empathize with your spouse’s pain? Congratulations, your depression is in remission! They’ve redefined mental health as emotional lobotomy and convinced us to celebrate our numbness as recovery.
Think about what this means for marriages: Your depressed spouse starts SSRIs, and within months they’re neurologically incapable of feeling your emotional pain. The researchers called this a “protective function,” but let’s call it what it really is: chemically-induced sociopathy. The study showed decreased connectivity between brain regions responsible for emotional and cognitive empathy. Translation: the drug literally disconnects the wiring that allows us to feel for each other.
The Anti-Human Agenda
Let’s call this what it is: an anti-human movement masquerading as mental health care. When you create drugs that systematically disable the neurochemical foundations of human bonding, empathy, and moral reasoning, you’re not treating illness; you’re engineering the dissolution of the social fabric itself.
But SSRIs are just one weapon in a much larger war against human flourishing. Look around: We’re poisoning masculinity as “toxic,” redefining female hormonal cycles as psychiatric disorders, and severing our children from nature itself, replacing dirt, sunlight, and real play with screens and synthetic environments. We’re feeding them processed poison disguised as food, then wondering why their bodies and minds rebel. We’re replacing human connection with digital interfaces, substituting virtual “friends” for real relationships, and celebrating isolation as “self-care.” Every institution that once fostered genuine human bonds (family, community, spiritual fellowship) is under systematic attack.
The gender confusion epidemic perfectly paralleling mass SSRI prescribing to adolescents? The explosion of young people who suddenly can’t recognize their own bodies, can’t connect to their biological reality? When you chemically sever a developing mind from its capacity to feel authentic connection to self and others, is it any wonder they become strangers in their own skin?
This anti-human agenda operates through multiple vectors: Seed oils inflaming our brains, endocrine disruptors scrambling our hormones, screens hijacking our attention, pornography replacing intimacy, and yes, psychiatric drugs severing our souls. Each element reinforces the others, creating a perfect storm of disconnection. The SSRIs ensure you won’t feel the horror of what’s being done to you. They’re the anesthesia for the operation that’s removing our humanity.
Every marriage destroyed by SSRI-induced apathy, every parent who stops feeling love for their children, every affair justified by chemically-induced emotional numbness: these aren’t unfortunate side effects. They’re features, not bugs, of a system designed to atomize human connection and create perpetual patients.
The online communities tracking this phenomenon aren’t conspiracy theorists or anti-medication extremists. They’re regular people sharing strikingly similar stories: My spouse started antidepressants and became someone else. They lost the ability to feel love. They rewrote our history. They destroyed our family with cold efficiency. And when they finally stopped the drugs (if they stopped) they woke up horrified at what they’d done.
One woman in these forums wrote something that haunts me: “The drug didn’t just steal my husband. It stole the person he was during our children’s most formative years. Even though he’s himself again now, off the drugs, our kids don’t know who he really is. They only know the emotionally absent stranger who lived in our house for three years.”
The Revolution We Need
The psychiatric establishment won’t save us from this; they created it. The therapists validating drug-distorted realities won’t help; they’re complicit. The only solution is brutal honesty about what these drugs actually do to human consciousness and connection.
If you’re on SSRIs and your marriage is falling apart, consider this: Maybe it’s not your marriage that’s broken. Maybe it’s your capacity to feel it.
If your partner started antidepressants and became a stranger, you’re not imagining it. You’re witnessing a chemically-induced personality transplant.
If you’re a therapist reading this and getting defensive, ask yourself: How many marriages have you helped validate into destruction because you couldn’t question the sacred cow of psychiatric medication?
We need to stop pretending that chemically altering the foundation of human emotion and connection is neutral. We need to stop acting like SSRIs are precision instruments when they’re actually neurochemical sledgehammers. We need to acknowledge that when you interfere with serotonin, you’re not just adjusting mood; you’re rewiring the capacity for love itself.
The families destroyed by SSRIs aren’t collateral damage; they’re casualties of an undeclared chemical war on human connection. And until we’re willing to name this war and fight back, the casualties will keep mounting, one numbed-out divorce at a time.
Your depression might be real. Your anxiety might be valid. Hell, in this toxic wasteland of a culture we’ve created, feeling depressed and anxious might be the only sane response. But look at how we’ve been programmed to address these legitimate feelings: Rush to the doctor. Get the diagnosis. Take the pill. Never once questioning whether numbing the pain is the same as healing it.
We’ve been brainwashed to believe that feeling less is the same as feeling better, that chemical numbness equals mental health. But is addressing your struggle this way worth sacrificing your capacity to love and be loved? Is it worth becoming a stranger to yourself and everyone who matters to you? Is a life without authentic emotional connection really better than a life with difficult emotions?
This more than a medical question. It’s a spiritual one. And the answer might just save your marriage and your soul.
RESIST
How Your Family Doc Became a Vaccine & Drug Enforcement Agent
The rise of pharmaceutical compliance officers in primary care
By Dr. Roger McFillin | Radically Genuine | Apr 3, 2025
Remember when your family doctor was actually your doctor? That quaint historical period when physicians made independent medical judgments instead of reading from pharmaceutical scripts? When they looked at you as a unique human being rather than a collection of compliance metrics needing correction?
Those days are fucking gone.
Today’s primary care physician is something entirely different—a pharmaceutical compliance officer with a prescription pad, a corporate protocol to follow, and overlords tracking their every move. They’ve transitioned from healers to hustlers, from medical professionals to medication pushers, from trusted advisors to glorified drug dealers with better parking.
I recently had a conversation with a pediatrician that exposed the naked truth of modern medicine. He confessed to me—with a mixture of resignation and discomfort—that he was “mandated” to administer the PHQ-9A (depression screening) to every adolescent, and if they scored above a certain threshold, he MUST offer an SSRI antidepressant.
“What if the teen is just going through a breakup or having normal adolescent mood swings?” I asked.
He shrugged helplessly. “Doesn’t matter. If they hit the number on the screening, protocol says I have to offer medication.”
“But you know these drugs more than double the risk of suicidal events in teenagers,” I pressed. “The black box warning exists for a reason.”
His response chilled me: “If something happened to the teen and I didn’t follow protocol—if I didn’t offer the medication—I could be held liable. My hands are tied.”
And there it was—the perfect analogy hiding in plain sight. This highly educated physician with years of training wasn’t making independent medical decisions. He was a street-level drug dealer who feared what would happen if he didn’t move enough product for his overlords. The corner pusher fears his supplier’s enforcers; the modern physician fears “liability” and “protocol violations.” Different vocabulary, identical dynamic.
Primary care has been transformed from a healing profession into a pharmaceutical distribution network with doctors serving as glorified vending machines in white coats. They’re the street-level dealers in the medical-industrial complex, pushing products with the ruthless efficiency of a cartel but with better branding and tax benefits.
The parallels between how primary care physicians push psychiatric drugs and vaccines are so perfect they deserve admiration from a purely marketing perspective. It’s the same hustle with different packaging—one comes in pill form, the other in a needle, but the script is identical.
The SSRI Hustle
God forbid you or a family member is unfortunate enough to schedule a routine checkup during a particularly bad week. Walk into that sterile exam room while grieving a loss, stressing about work, or just experiencing one of life’s inevitable rough patches, and you’ll walk out with a ‘mild to moderate depression’ diagnosis faster than you can say ‘pharmaceutical kickback.
Within minutes, you’re handed a questionnaire with loaded questions like: “Feeling bad about yourself or that you have let yourself or your family down or that you are a failure?” (You just watched your ex’s vacation photos on Instagram while eating ice cream for dinner in your unwashed sweatpants, so… is this a trick question?)
Answer honestly, and congratulations! You’ve just self-diagnosed with “mild to moderate depression.”
You mean what we used to call sad?
Your doctor spends approximately 90 seconds validating this with probing questions like “And how long have you felt this way?” before reaching for the prescription pad.
“I think Lexapro would really help take the edge off,” they say with practiced compassion, already halfway through writing the prescription. “It will balance your brain chemicals.”
But it’s when you express hesitation that the real sales pitch begins—fear. This is where doctors transform into pharmaceutical fear merchants:
“You know, untreated depression can be very serious,” they warn ominously. “It can worsen over time. It can affect your relationships, your work, your entire life. Depression is a serious medical condition—in fact, it’s the leading cause of disability worldwide.”
The implication hangs in the air like a guillotine blade: refuse this medication, and you’re gambling with your life. They may even pull out the suicide card: “Depression can lead to suicidal thoughts if left untreated.” The cosmic irony of using suicide as a scare tactic to prescribe drugs with black box warnings about increasing suicidal ideation seems lost on them.
For teenagers, the fear tactics are directed at parents. “You don’t want to take chances with your child’s mental health, do you?” they ask, making parents feel like monsters for questioning whether their teen’s temporary sadness requires a medication that doubles their risk of suicidal events.
This isn’t medical counseling. It’s emotional manipulation through fear—the same tactic used by predatory salespeople in every industry. “Better safe than sorry” becomes the catch-all dismissal of legitimate concerns about medications with profound risks and modest benefits.
What they don’t mention:
The “chemical imbalance” theory of depression was thoroughly debunked years ago, joining phrenology and bloodletting in medicine’s hall of shame. SSRIs have never proven to be clinically meaningful beyond placebo.
Complying with their prescription pad evangelism could result in permanent sexual dysfunction—as in forever, as in the rest of your life.
Withdrawal can be so brutal and protracted that patients often mistake it for “proof they need the medication” rather than recognizing it as drug dependence.
And here’s the cosmic punchline: in the 4-6 weeks it takes for these medications to supposedly “work,” most situational “depression” would have naturally improved anyway.
When that happens?
The doctor smugly nods and thinks, “See, the drugs I prescribed fixed them!” Never mind that time, human resilience, and your own natural healing did all the heavy lifting while the medication was just along for the expensive, side-effect-laden ride.
The Vaccine Hustle
Now let’s watch the vaccine version of the same performance:
You visit for a completely unrelated issue—perhaps a sprained ankle or a skin rash. Before addressing your actual concern, your doctor casually mentions, “I see you haven’t had your COVID or flu shot this year.”
The framing is already perfect—you’re “behind” on something, implying non-compliance with an expected standard. Your medical record has been flagged for a deficiency that needs correcting, like a car overdue for an oil change.
Express hesitation, and witness the same script unfold: “These vaccines are very safe and effective. Side effects are usually just a sore arm or mild fatigue for a day.” (Myocarditis? Menstrual disruptions? Neurological issues, complete hijacking of my immune system? Those are so rare they’re not worth mentioning, apparently.)
Ask about actual risk reduction—like how the flu vaccine isn’t efficacious and doesn’t prevent you from contracting the flu—and watch them shift uncomfortably.
Why would I even risk Guillain–Barré syndrome for this Doc? I am healthy and not that scared of the flu? Regardless of the low risk of complications… why even take that risk?
Dare to question whether a perfectly healthy 17-year-old who already recovered from COVID needs an experimental mRNA intervention that doesn’t prevent transmission—and has now been shown to actually INCREASE susceptibility to infection over time, not to mention the myocarditis risks, menstrual disruptions, and other “rare” side effects conveniently minimized in the sales pitch—and watch their face transform before your eyes.
First comes the reflexive smile-cramp, that frozen rictus of medical authority being questioned. Then the slightly widened eyes as they process your heretical departure from the script. Finally, that subtle hardening around the jaw as they shift from healthcare provider to pharmaceutical enforcement officer.
It’s like watching someone toggle between “friendly neighborhood doctor” and “COVID compliance commissar” in real-time, all because you had the audacity to weigh risks against benefits for your own child.
But regardless of whether they’re pushing pills or jabs, we see the identical sales pitch every time—a masterclass in pharmaceutical propaganda. They dramatically exaggerate even the most microscopic potential benefits while feverishly minimizing, dismissing, or flat-out denying any risks with the practiced ease of a seasoned con artist. Watch them transform a 1% absolute risk reduction into ‘90% effective!’ while simultaneously downgrading ‘known serious adverse events’ to ‘extremely rare side effects that aren’t worth discussing.’ It’s as if they’ve never read a single page of the actual scientific literature on the subject.
Spoiler alert: they haven’t.
Most haven’t ventured beyond industry-funded continuing education modules and pharmaceutical company press releases since medical school. The journal articles gathering dust in their mental libraries are pharmaceutical marketing materials disguised as science, cherry-picked datapoints that support the sales pitch while burying inconvenient truths beneath statistical sleight-of-hand. Their ‘expertise’ is just regurgitated talking points from the last drug rep who bought them lunch.
Your Doctor Now Reports to Corporate Masters
The corporate takeover of medicine didn’t happen overnight—it was systematically engineered, with the Affordable Care Act delivering the knockout blow to independent practice. While marketed as expanding “healthcare access,” Obamacare buried small practices under an avalanche of regulatory requirements, EHR mandates, and compliance costs that made independence financially impossible.
Before the ACA, over half of physicians owned their practices; today, that number has plummeted below 30%. The rest were forced to sell out to corporate healthcare systems where their compensation and job security now depend on following protocols—including pharmaceutical prescribing patterns and vaccination targets—established by administrators who’ve never touched a stethoscope.
Your family doctor didn’t willingly transform into a pharmaceutical enforcement agent; they were legislated into compliance, their medical autonomy sacrificed on the altar of corporatized healthcare while maintaining the illusion of independent judgment.
Primary care healthcare professionals are now following protocol with the unquestioning obedience of a first-grader desperate for a gold star sticker. It makes you wonder how many who flock to primary care medicine were those perfect little rule-followers their entire lives—the ones who color-coded their highlighters in medical school, memorized every algorithm without asking why, and spent their formative years as professional hoop-jumpers. The straight-A students who never risked a teacher’s disapproval, never colored outside the lines, never questioned authority figures even when those figures were demonstrably wrong. The ones whose entire identity became wrapped up in following instructions perfectly to achieve the next credential, the next white coat, the next professional validation.
Is it any surprise that these same personalities now cling to protocols like religious scripture, unable to exercise independent clinical judgment when a human being’s complex situation doesn’t fit neatly into their laminated flowchart? Critical thinking requires the courage to ask uncomfortable questions—a skill that was systematically extinguished in these pristine academic specimens long before they wrote their first prescription
Next time your primary care physician tries to prescribe you an SSRI for being human or jab you with the latest pharmaceutical subscription service, remember: you’re not a patient—you’re a customer they’re trying to upsell.
Their script may be polished, but your bullshit detector doesn’t need a medical degree to function properly. Ask the uncomfortable questions they’re afraid to answer. Demand actual data, not rehearsed talking points. Walk out if necessary.
Find the rare physicians who still practice medicine instead of pharmaceutical compliance. And if your doctor looks horrified when you decline their latest pill or shot, smile sweetly and say, “Don’t worry, I’ll make sure my chart notes that YOU failed to convince ME—not the other way around.”
After all, the most rebellious act in modern healthcare isn’t refusing treatment—it’s insisting on informed consent in a system designed to eliminate it.
Your body, your mind, your choice. No prescription required.
RESIST
Lawmakers say RFK Jr. is spreading misinformation about psychiatric drugs
The real threat may be their attempt to silence the debate
By Maryanne Demasi, PhD | April 9, 2025
The Make America Healthy Again (MAHA) Commission, established by Executive Order, convened its first meeting last month.
Among the topics discussed was the “threat posed by the prescription of selective serotonin reuptake inhibitors (SSRIs), antipsychotics, mood stabilisers, and stimulants.”
Shortly thereafter, a group of legislators issued a strongly worded letter to Health Secretary Robert F. Kennedy Jr, accusing him of “promoting disproven and outright false theories” about these medications—reframing them as “behavioral health medication.”
They argued that even suggesting these drugs might pose a “threat” would “stigmatize” Americans with mental health conditions and potentially deter them from seeking medical care.
But labelling something a “threat” in a policy discussion is not a condemnation; it is an invitation to assess risk—a fundamental responsibility of medical oversight.
The letter, led by Senator Tina Smith, urged Kennedy to “adhere to the well-established and widely accepted scientific and medical consensus” on the matter.
Consensus? This is precisely the problem—they are appealing to authority to shut down inquiry rather than fostering critical examination.
The FDA itself has placed a black box warning on SSRIs, cautioning that studies have shown these drugs double the risk of suicidal ideation and behaviour in certain populations.
Should that warning be revoked for fear of discouraging treatment?
Are we now at a point where simply discussing the risks of medications is considered dangerous? What happened to informed consent?
And if we are to insist on evidence – as the legislators say – where is their study that suggests educating people about the harms and benefits of medication prevents them from seeking treatment?
It does not exist.
In many cases, psychotherapy should be prioritised over medication, as it is safer, more effective in the long run, and aligns with what most patients prefer.
Neither the MAHA Commission nor Kennedy has advocated for anyone to stop taking medication abruptly—a well-known risk—but rather to investigate the full scope of these drugs’ effects.
The legislators cited CDC statistics showing that “43 percent of children between the ages of 3 and 17 took medication for an emotional, concentrational, or behavioral condition,” then immediately noted that “youth mental health needs have only increased in the past five years.”
The contradiction is glaring—if these medications were the solution, why is the problem worsening? This is precisely what Kennedy seeks to investigate.
One of the most contentious points was Kennedy’s claim that SSRIs have been linked to school shootings in the U.S.
The legislators cited studies such as an analysis of FBI data on “educational shootings” from 2000-2017, which concluded that the majority of school shooters had not been previously treated with psychotropic medication.
However, these data are incomplete. Privacy laws restrict access to shooters’ full medical histories, making definitive conclusions about many of these analyses difficult.
Meanwhile, a 2015 study published in PLOS One by Moore et al. found a disproportionate association between certain psychotropic drugs and violent behaviour in the FDA’s adverse event reporting system.
The harms of antidepressants are often downplayed—even in the medical literature.
Comparisons between published studies and confidential regulatory documents have revealed significant discrepancies, including underreporting of suicide attempts and aggressive behaviour.
My point is, Kennedy is not asserting causation—he is calling for more research. The legislators’ dismissal of his concerns as “disproven” serves only to suppress an important discussion that demands further scrutiny.
At his confirmation hearing, Kennedy remarked, “I know people, including members of my family, who’ve had a much worse time getting off of SSRIs than getting off of heroin.”
Legislators strongly objected to the comparison in the letter, but Kennedy was referring to the well-documented difficulties of SSRI discontinuation—affecting about half of those who take them, even though their dependency profile differs from that of opioids.
What most people don’t realise is that psychiatrists who specialise in tapering patients off antidepressants report that SSRI-withdrawal can last far longer than withdrawal from heroin.
In fact, some patients remain on SSRIs indefinitely—not by choice, but because withdrawal symptoms are so severe that stopping is unbearable. The legislators’ letter conveniently ignores this reality.
Instead of engaging with the substance of his arguments, Kennedy’s critics attacked his qualifications, claiming he was “unqualified” to weigh in on mental health or addiction.
True, Kennedy is not a psychiatrist—or even a physician. But as a lawyer who has spent decades exposing the failures of public health institutions, he understands where scrutiny is needed.
Moreover, Kennedy is not issuing medical directives—he is demanding accountability in a system that too often fails to critically examine the long-term effects of the medications it prescribes.
As Danish physician Peter Gøtzsche has shown, prescription drugs are a leading cause of death, surpassing even heart disease and cancer—and psychiatric medications alone are the third leading cause of death.
Why are these legislators so adamantly defending what is widely acknowledged as the rampant over-prescription of psychiatric drugs? Could it have anything to do with their deep ties to Big Pharma lobbyists?
Their eagerness to silence dissent suggests that the interests being protected may not be those of the public, but rather those of the industry that funds their campaigns.
I have been writing about this issue for years, exposing the pharmaceutical industry’s role in shaping narratives around psychiatric drugs while downplaying their harms.
The pattern is always the same — suppress uncomfortable discussions, attack those who raise legitimate concerns, and protect the status quo.
How fragile do these legislators think people are, that they shouldn’t be trusted with the full truth about the medications they take? And more disturbingly, what gives them the authority to control what information the public is allowed to access?
Kennedy pledged that “nothing is going to be off limits” in his effort to Make America Healthy Again—this is what he meant.
Raising questions is not misinformation. And shutting down debate is not science.
If policymakers are confident in the safety and efficacy of these drugs, they should welcome scrutiny—not suppress it.
Below is a letter from Kim Witczak, a drug safety advocate – addressed to Senator Tina Smith. It requests a meeting to discuss mental health and antidepressant safety concerns, referencing Witczak’s personal experience, attaching 15 studies highlighting issues like clinical trial misconduct and regulatory failures


How Antidepressants Are Numbing More Than Depression
The devastating effects on empathy, love, intimacy & sex
By Dr. Roger McFillin | Radically Genuine | August 15, 2024
In our relentless pursuit to transcend the human suffering, we’ve stumbled into a dangerous oversimplification: an improved mental state reflects the absence or decrease in negative emotional states. This reductionist view has not only cheapened our understanding of the human emotional spectrum but has also paved the way for a troubling linguistic shift.
The word “sad” has all but vanished from our lexicon, replaced by the catch-all term “depression” – a linguistic sleight of hand that medicalizes every shade of human sorrow, from loneliness to anxiety, from fear to disappointment. This semantic broadening has opened the floodgates for indiscriminate prescribing of “antidepressant” drugs, extending far beyond their original purpose to treat clinical depression.
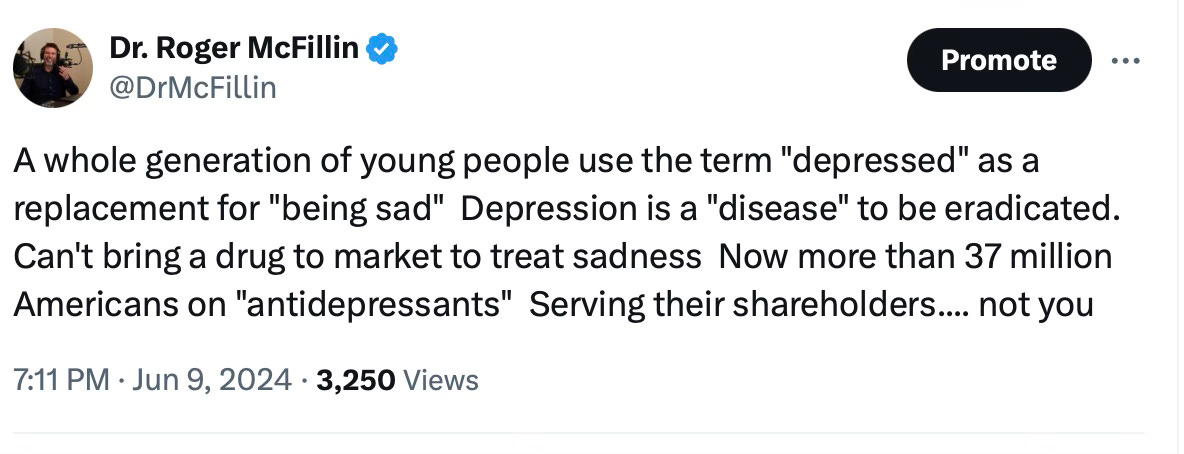
Today, these powerful drugs are doled out for an alarming array of off-label conditions: gastrointestinal issues, fibromyalgia, grief, chronic pain, and eating disorders, to name but a few. This prescription epidemic is built not on scientific evidence, but on a dangerous myth – the allure of a quick fix for life’s complexities. The medical profession and mental health communities, seemingly hypnotized by the promise of “antidepressant” effects, have unwittingly become complicit in a grand experiment on human neurochemistry.
At the heart of this phenomenon lies a disturbing paradox: the very mechanism that gives these drugs their “antidepressant” label – emotional blunting – is causing more harm than good. By dampening our ability to feel, these “medications” offer a Faustian bargain: potential short-term relief from suffering at the cost of our full range of human experiences.
For those battling severe clinical depression, the trade-off of emotional blunting might seem a necessary evil. Yet paradoxically, these individuals often struggle most acutely with the very emptiness that antidepressants can exacerbate. More alarmingly, the vast majority caught up in the widening net of antidepressant prescriptions aren’t facing such severe depressive episodes. For them, the potential for permanent emotional deadening was never a consideration, let alone a risk they knowingly accepted.
Emotional Blunting is Not Mental Healthcare
In our misguided quest to eradicate pain, we’ve stumbled upon a chemical lobotomy that threatens the very essence of what makes us human. Emotional blunting, the insidious “side effect of antidepressants”, doesn’t just dull our sorrows – it extinguishes the vibrant flames of joy, love, and connection that give life its meaning.
Imagine a world painted in shades of gray, where the highs of ecstasy and the lows of despair are replaced by a monotonous, tepid middle ground. This is the reality for countless individuals trapped in the purgatory of SSRI-induced emotional blunting. They walk through life as spectators, unable to fully participate in the rich tapestry of human experience.
The medical establishment, in its haste to silence the symptoms, has forgotten a fundamental truth: pain, in all its forms, is not just an inconvenience to be eliminated. It’s a vital signal, a call to action, a catalyst for growth and change. By indiscriminately muting this signal, we’re not just treating depression – we’re risking the very essence of what makes us human.
But the consequences of this chemical flattening extend far beyond personal discomfort. Recent research has unveiled a chilling truth: SSRIs decrease affective empathy, our ability to emotionally resonate with others’ experiences. Neuroimaging reveals a reduction in activity across three crucial brain regions associated with empathy for pain. In our attempt to shield ourselves from suffering, we’ve created a generation of emotional zombies, incapable of truly connecting with the joys and sorrows of those around them.
Consider the implications for love and attachment – the very foundations of human society. How can one form deep, meaningful bonds when the heart’s strings have been chemically severed? The butterflies of new love, the warmth of familial affection, the bittersweet ache of nostalgia – all reduced to mere concepts, intellectually understood but never truly felt. In this emotional wasteland, how can we expect individuals to develop a robust sense of gender and sexual identity, both of which are intimately tied to our capacity for emotional and physical intimacy?
The cruel irony is that in our desperate bid to numb pain, we’ve numbed everything that makes life worth living. Joy becomes a faded memory, a concept understood but no longer experienced. The exhilaration of achievement, the quiet satisfaction of a beautiful sunset, the overwhelming surge of love for a newborn child – all diluted into pale imitations of their former glory.
This emotional castration strikes at the very heart of the human spirit. Our ability to feel deeply – to be moved by music, stirred by art, inspired by acts of kindness – is what separates us from machines. It’s the wellspring of creativity, the driving force behind innovation, the fuel for compassion and altruism. By chemically muting these essential aspects of our humanity, we risk creating a society of hollow individuals, going through the motions of life without ever truly living.
The consequences ripple out far beyond the individual. A populace incapable of deep emotional resonance is a populace ripe for manipulation, apathy, and moral decay. How can we expect people to fight injustice, to stand up for the oppressed, to sacrifice for the greater good, when they can no longer feel the burning indignation or overwhelming compassion that drives such actions?
In our shortsighted attempt to eliminate suffering, we’ve stumbled upon a cure far worse than the disease. The price of emotional blunting is nothing less than our humanity itself. As we continue down this perilous path, we must ask ourselves: in our quest for painlessness, are we willing to sacrifice everything that makes us human? What impact does this emotional blunting have on sexual desire and intimacy?
Post SSRI Sexual Dysfunction (PSSD)
Imagine a world where the very essence of your being – your capacity for intimacy, pleasure, and connection – is suddenly and inexplicably stripped away. This isn’t the plot of a dystopian novel; it’s the harsh reality for countless individuals suffering with Post-SSRI Sexual Dysfunction (PSSD), a hidden epidemic born from our society’s pill-popping approach to mental health.
A vibrant libido isn’t just about carnal pleasure; it’s the body’s barometer of vitality, a complex symphony of physical, hormonal, and psychological factors humming in harmony. But for those struck by PSSD, this life-affirming melody is replaced by a deafening silence.
PSSD is the pharmaceutical industry’s dirty little secret, a Pandora’s box of sexual side effects that persist long after the last antidepressant pill is swallowed. We’re talking about a cruel trifecta of desire destroyed, genitals numbed, and an inability to orgasm.
The numbers are staggering – up to 73% of patients dancing with these serotonin-enhancing devils report one or more of these bedroom-killing effects. That’s not a side effect; that’s a full-blown assault on human sexuality.
But here’s where it gets truly Kafkaesque: PSSD doesn’t play by the rules. It doesn’t fade away when you kick the meds to the curb. No, it sets up shop in your nervous system, potentially rewiring your sexual circuitry for years – or even indefinitely. Imagine trying to rebuild your life post-depression, only to find that your capacity for one of life’s most fundamental joys has been carpet-bombed into oblivion.
The medical community, in its infinite wisdom, largely turns a blind eye to this sexual holocaust. PSSD sufferers are left adrift in a sea of misdiagnoses and dismissals, their anguish compounded by the very professionals sworn to help them.
As for the root cause of this sexual sabotage? The jury’s still out. Some point to a chemical lobotomy of the brain’s pleasure centers, others to a genetic vandalism that silences the body’s sexual whispers. But while the white coats scratch their heads, real people are left struggling with shattered relationships, crippled self-esteem, and a quality of life that’s been gutted like a fish.
We stand at a critical juncture in mental health care, facing a silent epidemic that threatens the very essence of human experience. Post-SSRI Sexual Dysfunction (PSSD) is not just a side effect – it’s a life sentence of emotional and sexual numbness that demands immediate recognition and action.
To the medical community, pharmaceutical industry, and mental health advocates: I implore you to acknowledge PSSD as a real and devastating condition. To researchers and funding bodies: We desperately need your support to unravel the mechanisms behind PSSD and develop effective treatments. Donations could be the lifeline that restores hope to countless sufferers.
But recognition and research are not enough. We must revolutionize the informed consent process for antidepressant prescription. To every potential patient, we pose this grave question:
Would you willingly sacrifice your ability to feel emotions deeply, to experience sexual desire, and to forge intimate connections, all for the possibility of short-term relief?
This is not a hypothetical – it’s the reality faced by PSSD sufferers worldwide. We demand transparency about these risks before a single pill is prescribed. The human cost of our current approach is too high, the potential for lifelong suffering too great. It’s time to prioritize true informed consent and explore alternative treatments that don’t gamble with the core of our humanity. The stakes couldn’t be higher – it’s not just about saving lives, but preserving what makes those lives worth living.
I encourage everyone to visit the PSSD Network to learn more about this debilitating condition.
TUCKER CARLSON ON OPIOIDS, COVID AND ANTIDEPRESSANTS
TUCKER CARLSON TONIGHT | JULY 25, 2022
Tucker Carlson reveals the shocking side effects of antidepressants and calls out Democrats for not holding Big Pharma accountable. His full opinion piece can be read here: https://www.foxnews.com/opinion/tucker-carlson-drugs-not-answer-every-human-problem


