The Streetlight Effect
Lies Are Unbekoming |January 31, 2026
What
The vaccinated versus unvaccinated study does not exist.
Not “hasn’t been done well.” Not “needs more funding.” Does not exist. No large-scale, long-term study has ever compared total health outcomes of vaccinated children against those who received no vaccines at all. The most basic question a parent might ask—what happens to children who get the full schedule versus children who get none of it?—has never been answered.
The tampon-cervical cancer study does not exist.
Women insert products containing lead, arsenic, cadmium, dioxins, and PFAS directly against cervical tissue, for days each month, for decades. The vaginal epithelium absorbs substances more efficiently than swallowing them—pharmaceutical companies exploit this property deliberately. No study has examined whether this chemical exposure causes the cancer that develops in that tissue.
The long-term antidepressant outcome study does not exist.
Millions take SSRIs for decades. No study has followed patients long enough to determine whether these drugs improve life outcomes compared to people who experienced similar depression but did not take them.
These are not gaps in the research. These are the research.
The streetlight effect takes its name from an old joke. A drunk searches for his keys under a streetlight. A policeman asks where he dropped them. “In the bushes,” the drunk says. “Then why are you looking here?” “Because this is where the light is.”
The joke works because the behaviour is absurd. No one would search where they know the answer isn’t, simply because that’s where they can see.
Except institutions do exactly this. Every day. As policy.
The streetlight effect, as it operates in captured institutions, is not cognitive error. It is not researchers making innocent mistakes. It is the deliberate positioning of the light to ensure certain questions are never asked and certain answers are never found.
This is not censorship. Censorship is visible, resistible, galvanizing. The streetlight effect is invisible. The scientist who never receives funding for the destabilizing question does not experience suppression—they experience a career that simply moved in other directions. The question dies without ever being asked. The ignorance is architecturally produced.
Peter Duke (The Duke Report™️) calls this epistemic warfare—the deliberate construction of ignorance as a strategic weapon. The battlefield is what you’re allowed to know.
The drunk in the joke is stupid. The people positioning the lampposts are not.
The Machine
The streetlight effect does not operate alone. It is one component in a larger machine that creates stable falsehood.
Consider a pole balanced perfectly vertical. This represents truth in equilibrium. It requires no energy to maintain—gravity holds it in place. Now tilt the pole twenty degrees from vertical. Enormous energy must flow into the base to prevent collapse. Struts, supports, constant adjustment. A partial deviation from truth demands perpetual maintenance.
But invert the pole completely—one hundred eighty degrees—and it balances again. Not because it has escaped gravity, but because the inversion is complete enough to create its own coherent structure. A partial lie must argue with reality. A complete inversion replaces reality. The internal logic becomes consistent, even though every element points in the wrong direction.
This is how medical orthodoxy maintains itself. The cholesterol hypothesis, the viral theory of disease, the vaccine safety consensus—these are not partial deviations requiring constant defense. They are complete inversions that have found their own equilibrium. Once trillions of dollars of infrastructure are built around the inverted pole—careers, institutions, industries, identities—the structure stands for generations.
The streetlight effect is what keeps the inversion stable. It ensures the studies that would expose the inversion never get funded. The questions that would topple the pole never get asked. The light shines where the answers aren’t, and the darkness protects what cannot survive scrutiny.
The Components
The founding lie. Every inversion begins with a deliberate decision to construct a reality opposite to truth. Someone knows the truth and chooses to build the inversion. The tobacco executives who wrote “doubt is our product” in 1953. Ancel Keys selecting six countries from twenty-two. Simon Flexner declaring viral causation without demonstrating any virus. The founding lie need not be elaborate—it needs only to be simple enough to anchor a heuristic and complete enough to form a coherent alternative.
Epistemic capture. The systematic colonization of institutions that produce and validate knowledge. Journals, regulatory bodies, funding agencies, medical schools. When captured, the inversion gains legitimacy. It becomes “the science” rather than a lie being told. Two-thirds of medical school department chairs have financial ties to pharmaceutical companies. Two-thirds of researchers carry conflicts of interest. The top two-thirds of universities own pharmaceutical stock. Most clinical trials are conducted by for-profit Contract Research Organizations. Up to 40% of medical journal articles are ghostwritten by the industry. The $27 billion spent annually on drug promotion exceeds the entire NIH budget. Capture this system and you capture the epistemology of the entire society. The inversion no longer needs to persuade—it certifies.
The herd-mind limitation. Collective cognition cannot perform slow thinking. It holds only simple heuristics—two-variable formulas compressing reality into actionable shortcuts. “Cholesterol causes heart disease; statins prevent it.” “Viruses cause illness; vaccines prevent it.” “HPV causes cancer; Gardasil prevents it.” Two variables, one relationship. This is not stupidity—individuals can think slowly and hold multiple variables. But the collective runs on pattern-matching shortcuts. Whoever installs the two anchor points controls the collective understanding. The streetlight effect ensures no competing formula can form, because the evidence that would generate it remains in darkness.
The complicity of comfort. The inversion succeeds not only because institutions enforce it but because populations prefer it. A comfortable lie demands nothing. An uncomfortable truth demands everything—action, disruption, reversal of past choices, separation from the herd. The parent who accepts that vaccines are safe can believe they protected their child. The parent who questions must face what they may have done, and must find the courage to refuse the next injection while doctor, family, and social circle apply pressure. The comfortable lie offers belonging. The uncomfortable truth offers exile. Given the choice, most people choose comfort. They are not stupid. They are human. The inversion exploits this.
Convergent opportunism. Once the inversion is seeded, other actors discover the structure serves them. They join maintenance without coordination. Pharmaceutical companies profit from the products the inversion protects. Doctors maintain income and status by following captured protocols. Regulators secure future employment by approving what industry wants approved. Journals collect advertising revenue and reprint fees. Academic careers are built on the approved research agenda. Politicians receive donations. Media companies receive advertising. No one needs to be in a room together. Their interests converge on the same structure like iron filings around a magnet. The original architects can retire or die. The founding lie no longer requires their maintenance. The ecosystem maintains itself.
The streetlight effect. Research, funding, and career advancement concentrate in the illuminated zone. Questions that would destabilize the inversion lie in darkness—not forbidden, merely unrewarded. Scientists go where the light is. The ignorance is architecturally produced.
The components interlock. Epistemic capture makes the heuristic installation possible—the two anchor points are certified as “settled science.” The herd-mind limitation makes capture effective—the collective cannot audit the institutions it trusts. The complicity of comfort ensures the collective does not want to audit them—the truth is too costly. Convergent opportunism maintains the streetlight—each actor has incentive to keep the illuminated zone stable. The streetlight produces the ignorance that protects the founding lie from scrutiny. No central control required. Each component creates conditions for the others.
How the Light Gets Positioned
Funding control. Fund what you want studied. Don’t fund what you don’t want studied. A study that doesn’t exist cannot produce inconvenient findings.
Definitional control. Define questions narrowly enough that desired answers become inevitable. Define vaccine safety as “does not cause the specific harm we’re testing for in the short window we’re testing,” and you can find vaccines safe while ignoring every harm you didn’t test for. Define “isolation” as detecting genetic sequences rather than extracting particles, and you can claim viruses are isolated without ever demonstrating they exist.
Methodological control. Use active comparators instead of inert placebos. The HPV vaccine trials used aluminum adjuvant as the “placebo”—a toxic substance guaranteeing the control group would experience adverse events. Exclude participants likely to have adverse reactions. End trials before long-term effects appear. Choose surrogate endpoints instead of outcomes that matter.
Publication control. Fund journals, sit on editorial boards, peer review each other’s papers. Authors with conflicts of interest are twenty times less likely to publish negative findings. The Lancet generates up to two million euros from reprints when a positive drug study is published. The same investment funds—BlackRock, Vanguard—that own major pharmaceutical stakes also own the journals that evaluate their products. Publish what supports the narrative. A finding that isn’t published doesn’t enter “the scientific consensus.”
Career control. Reward researchers who produce useful findings. Punish those who produce threatening ones. Kilmer McCully discovered homocysteine—his laboratory was moved to the basement, his funding evaporated, no institution would hire him for two years. The survivors learned what questions not to ask. Upton Sinclair identified the mechanism: “It is difficult to get a man to understand something when his salary depends on his not understanding it.” Mortgages create beliefs.
Narrative control. Establish “scientific consensus” through the mechanisms above, then use it as a weapon. Anyone who questions it is “anti-science.” The lamppost is defended by making it socially impossible to point out it’s in the wrong place.
Once you begin, you cannot stop. The streetlight effect is not a one-time decision but continuous operation. Every year, researchers must be funded for approved questions and not funded for forbidden ones. Every year, journals must publish approved findings and reject threatening ones. The moment you stop, someone asks the forbidden question, funds the forbidden study, publishes the forbidden finding. This is why captured institutions respond to challenges with ferocity. A question that might move the lamppost threatens the entire inverted structure—because for the people who positioned the lamp, it does.
Why
Money is the mechanism. Power is the motive. Extraction is the outcome.
Control what questions get asked and you control what answers are possible. The chain is short: control what is studied → control what is known → control what is believed → control what is done.
The streetlight effect is infrastructure for extraction. You cannot build a system that extracts wealth through manufactured illness if people can see what is causing the illness. The lamppost must be positioned away from the cause before the extraction pipeline can operate. Shine the light on claimed viruses, genes, bad luck. Leave toxins, chemicals, iatrogenic injury in darkness. Attribute illness to nature rather than industry. The treatment becomes drugs rather than removal of harm. The patient becomes a customer. The extraction runs indefinitely.
The streetlight effect is not a bug in the system of knowledge production. It is the system.
The HPV Case
In 2006, journalists Torsten Engelbrecht and Claus Köhnlein contacted the German Cancer Research Centre—the DKFZ, one of the world’s leading cancer institutions—with four requests:
A study proving HPV exists through proper isolation.
A study proving HPV causes cervical cancer.
A study proving non-viral factors can be excluded as primary causes.
A study proving HPV vaccines are safe and effective.
The DKFZ provided literature for requests one, two, and four—though what they called “isolation” for request one was not isolation in any meaningful scientific sense. It was detection of genetic material declared viral without demonstrating that any virus existed. No particle was extracted from human tissue, purified, and shown to cause disease. The methodology assumes what it claims to prove.
For request three, they provided nothing.
This is the streetlight effect in its pure form. The question “could something other than the claimed virus cause this cancer?” was never investigated. Not because it was asked and answered. Because it was never asked. The light was positioned on virology from the start. Toxicology remained in darkness.
The statistics expose the positioning. Up to 80% of women test positive for HPV markers at some point. Less than 1% develop cervical cancer. In Germany, 0.017% of women develop cervical cancer annually. The marker is nearly universal. The disease is rare. If the marker caused the disease, the pattern would be different.
The establishment response is not to investigate what actually causes the cancer. The response is to add qualifiers—HPV is “necessary but not sufficient,” cofactors are required. The cofactors are vague enough to explain any distribution of cases: “immune status,” “genetic susceptibility,” “lifestyle factors.” The theory cannot be falsified because it absorbs any evidence. This is the hallmark of a stable inversion—internal coherence maintained by excluding the data that would destroy it.
Meanwhile, the chemical hypothesis sits in darkness, unstudied.
In 2024, researchers published the first study measuring metal concentrations in tampons. They found lead in every sample tested—at concentrations ten times higher than maximum levels allowed in drinking water. Arsenic in 95% of samples. Cadmium in 100%. Dioxins from chlorine bleaching. PFAS in products marketed as “organic” and “natural.”
The average woman who menstruates uses approximately 11,000 tampons over her reproductive lifetime. Each remains in contact with vaginal mucosa for hours. The vaginal epithelium is not a barrier; it is a gateway—pharmaceutical companies use vaginal administration precisely because it delivers substances to the body more efficiently than swallowing them.
Fifty years of cumulative exposure to documented carcinogens, delivered directly to the tissue where the cancer develops. The research examining this exposure as a cause of cervical cancer does not exist.
The mutation patterns found in HPV-negative cervical cancers—TP53, KRAS, PTEN, ARID1A—are consistent with chemical-induced DNA damage. The cancers that don’t fit the viral story fit the chemical story. No one is funded to look.
The HPV vaccine trials used aluminum adjuvant as the “placebo”—a toxic substance that guaranteed the control group would experience adverse events, making the vaccine appear safe by comparison. The trials never established whether the vaccine prevents cancer; they used surrogate endpoints and ended before cancer could develop. The protection claimed wears off before women reach the age when cervical cancer typically occurs.
The entire apparatus—causation claim, screening program, vaccine—is built on a lamppost positioned to illuminate virology and leave toxicology in darkness. The studies that would challenge this positioning do not exist. The questions that would threaten vaccine revenue do not get asked.
The founding lie. The captured institutions. The simple formula. The comfortable belief. The convergent interests. The positioned light. All the components, interlocking. The machine runs.
The Polio Precedent
The HPV case is contemporary. The pattern is not new.
In 1907, Simon Flexner of the Rockefeller Institute claimed to have isolated a poliovirus. His method: inject diseased human spinal cord tissue into monkey brains. When monkeys became ill, inject their tissue into other monkeys. Declare that whatever caused the illness must be a virus.
Flexner admitted in his 1909 paper that he “failed utterly to discover bacteria” and could not demonstrate any pathogen under the microscope. His conclusion: the agent “belongs to the class of the minute and filterable viruses that have not thus far been demonstrated with certainty.”
He could not demonstrate any virus. He concluded one must exist anyway—because he found no other explanation. He did not look for other explanations. He did not investigate toxins. He assumed viral causation and built an empire on the assumption.
The Rockefeller Institute was not a neutral scientific body. It was an instrument of Rockefeller interests—specifically, the interest in redirecting American medicine toward patentable drugs. In 1911, the Institute succeeded in having poliomyelitis entered into US Public Health Law as “a contagious, infectious disease caused by an air-borne virus.” No proof of contagion existed. No proof of any virus existed. Children with the disease kept in general hospital wards did not infect other patients. The law said it was contagious anyway.
By classifying poliomyelitis as viral, the Rockefeller Institute cut off investigation of alternatives. The lamppost was positioned. Toxicology was in darkness.
Then came DDT.
After World War II, DDT was released for civilian use, declared safe for humans. Cities sprayed beaches and swimming pools. Housewives sprayed kitchens and children’s mattresses. Farmers sprayed crops and dairy cows. From 1945 through 1952, US DDT production increased tenfold.
Polio cases increased in parallel. From 25,000 in 1943 to over 280,000 in 1952.
Dr. Morton Biskind testified to Congress in 1950, documenting over 200 cases where severe symptoms—including paralysis—disappeared when DDT exposure was eliminated. Dr. Ralph Scobey noted that polio symptoms matched known toxic poisoning patterns and that hospital polio wards never saw transmission between patients.
The Rockefeller-controlled National Foundation for Infantile Paralysis rejected this evidence. They funded vaccine research instead.
Beginning in 1951, as DDT use declined amid public concern and livestock deaths, polio cases fell by two-thirds—well before the Salk vaccine was widely administered. The decline tracked DDT reduction, not vaccine introduction.
The vaccine was credited anyway. The streetlight effect operated for decades, protecting the viral hypothesis from toxicological evidence.
Beyond Medicine
The streetlight effect operates wherever institutions benefit from not knowing.
LeBron James has played professional basketball for over twenty years. During that time, footage has accumulated showing him grabbing referees, screaming profanities in officials’ faces, flopping theatrically, committing uncalled fouls—each action a violation that would result in ejection or fines for other players. The footage is not hidden. It happens on national television, in real time, in front of millions of viewers.
ESPN does not report on it.
The same ESPN that posts about a player wearing an armband—content so trivial it borders on self-parody—does not mention a player grabbing a referee. No memo is required. ESPN holds broadcast rights to the NBA worth billions. They are not journalists covering the league; they are partners with the league. A reporter who runs that story damages their access. An editor who approves it damages their network’s relationship. Everyone understands what’s expected. The silence self-organizes.
The league benefits. The network benefits. The player benefits. The advertisers benefit. No coordination required. Each actor maintains their piece of the structure, and the pieces interlock without a blueprint.
The Lakers have led the NBA in free throw differential for four consecutive seasons. No other team has appeared in the top three more than once during that span. Their cumulative differential over those four years is +1,200. No other team has reached even +500. The numbers are public. The pattern is measurable. The coverage does not mention it.
The evidence is on screen. The media controls where the light of attention shines. Highlights are illuminated. Uncalled fouls happen in peripheral vision. Preferential treatment registers as background noise. People aren’t failing to see. They’re searching where they’ve been trained to search.
The Cholesterol Case
In 1852, Austrian pathologist Karl von Rokitansky proposed that atherosclerotic plaques were remnants of blood clots. He had performed thousands of autopsies and noticed that plaques looked exactly like clots in various stages of organization. The thrombogenic hypothesis—heart disease caused by clotting, not cholesterol accumulation—had compelling evidence from the start.
A century later, Ancel Keys positioned the lamppost elsewhere.
In 1953, Keys published a graph showing correlation between fat consumption and heart disease deaths in six countries. The points lay almost perfectly on a line. Data was available from twenty-two countries. Keys chose six. When Yerushalmy and Hilleboe analyzed all twenty-two countries in 1957, the correlation vanished.
The lamppost was positioned anyway.
The sugar industry recognized the threat. In the 1960s, researchers were linking sugar consumption to heart disease. The Sugar Research Foundation paid Harvard researchers the equivalent of $50,000 to write a review attacking anti-sugar studies while promoting the fat hypothesis. The researchers assured executives they were “well aware of your particular interest.”
The debate about sugar died. The war on fat intensified. The processed food industry could now replace expensive animal fats with cheap vegetable oils and sugar while marketing their products as “heart-healthy.”
Kilmer McCully discovered that homocysteine, not cholesterol, was destroying arteries. Children with genetic disorders causing high homocysteine developed severe atherosclerosis and died of heart attacks—despite normal cholesterol. McCully published his findings. Despite Harvard credentials and compelling evidence, he lost his position. His laboratory was moved to the basement. His funding evaporated. For two years, no institution would hire him.
The Framingham Heart Study, the longest-running cardiovascular study in history, produced a finding buried deep in its thirty-year report: “For each 1 mg/dl drop in cholesterol, there was an 11% increase in coronary and total mortality.” People whose cholesterol decreased were more likely to die. The study’s director later admitted: “In Framingham, the more saturated fat one ate, the more cholesterol one ate, the more calories one ate, the lower the person’s serum cholesterol.”
This contradicted everything the study was cited to support. The finding was not publicized.
Statins generate over $20 billion annually. The University of British Columbia’s Therapeutics Initiative concluded: “Statins have not been shown to provide an overall health benefit in primary prevention trials.” People without existing heart disease who take statins are no less likely to die.
The lamppost remains on cholesterol. The questions about clotting, sugar, homocysteine, stress, and metabolic dysfunction remain in darkness. Rokitansky’s thrombogenic hypothesis—supported by 170 years of autopsy evidence—sits unstudied while billions flow into cholesterol research. The studies that would move the light do not get funded. The researchers who ask the wrong questions do not get hired.
Seventy years. Billions of prescriptions. The founding lie. The captured institutions. The simple formula. The comfortable belief. The convergent interests. The positioned light. The same architecture.
Seeing the Lamp
The streetlight effect leaves signatures.
The absent study. A question any reasonable person would want answered, never investigated. The vaccinated-versus-unvaccinated comparison. The tampon-cancer link. The long-term antidepressant outcomes. When obvious questions remain unasked, ask who benefits from not knowing.
The aggressive defence. When someone asks the forbidden question, the response is not engagement but destruction—career attacks, accusations of conspiracy thinking, demands for retraction. Institutions confident in their evidence respond with evidence. Institutions defending a positioned lamppost respond with force.
The unfalsifiable theory. When a theory absorbs any contradictory evidence—when exceptions are explained away with cofactors, when it cannot specify conditions under which it would be proven wrong—you are looking at narrative maintenance, not science. You are looking at a stable inversion.
The funding trail. Who paid for the studies that exist? Who would have paid for the studies that don’t exist? The asymmetry reveals where the lamppost stands.
The career pattern. Who prospers in the field? Who disappears? When researchers who produce industry-friendly findings rise while researchers who produce threatening findings lose funding, laboratory space, positions—the incentive structure is visible.
The simple formula. When complex reality is compressed into two variables and one relationship—cholesterol causes heart disease, viruses cause illness, vaccines prevent disease—ask who installed the formula and who profits from it.
The comfort test. Does the official position demand anything of you, or does it offer easy absolution? The comfortable lie asks nothing. The uncomfortable truth asks everything.
The system depends on trust. Trust in institutions. Trust in expertise. Trust that the questions being asked are the right questions and the absence of other questions is innocent.
The streetlight effect ends when enough people start asking different questions. Why isn’t there a study on that? Who decided not to fund it? What would we find if someone looked in the dark?
The drunk searching under the streetlight is a figure of comedy. The institutions searching only where their funders want them to look are not funny.
They are why children receive vaccines never tested against unvaccinated controls.
They are why women develop cancers from products no one investigated.
They are why treatments that might work are never studied while treatments that profit the right people are studied endlessly.
The lamppost was positioned. It can be repositioned. But first you have to see it—and see the machine it is part of.
The next time you hear “no studies show,” ask the next question.
Who made sure those studies don’t exist?
That’s where the keys are.
References
HPV and Cervical Cancer
Engelbrecht, Torsten and Köhnlein, Claus. Virus Mania: How the Medical Industry Continually Invents Epidemics, Making Billion-Dollar Profits at Our Expense. Trafford Publishing, 2007.
Holland, Mary, Mack Rosenberg, Kim, and Iorio, Eileen. The HPV Vaccine on Trial: Seeking Justice for a Generation Betrayed. Skyhorse Publishing, 2018.
German Cancer Research Centre (DKFZ). Email correspondence with Engelbrecht and Köhnlein, October-December 2006.
Shearston, J.A. et al. “Tampons as a source of exposure to metal(loid)s.” Environment International, 190, 108849, 2024.
Marroquin, J. et al. “Chemicals in menstrual products: A systematic review.” BJOG: An International Journal of Obstetrics and Gynaecology, 131(5), 655-664, 2024.
Lee, Kwang-Beom et al. “Untold story of human cervical cancers: HPV-negative cervical cancer.” BMC Cancer, 2022.
Polio and DDT
Flexner, Simon and Lewis, Paul A. “The Transmission of Acute Poliomyelitis to Monkeys.” Journal of the American Medical Association, 1909.
Flexner, Simon and Lewis, Paul A. “The Nature of the Virus of Epidemic Poliomyelitis.” Journal of the American Medical Association, December 1909.
Biskind, Morton S. “Statement on Clinical Intoxication from DDT and Other New Insecticides.” Journal of Insurance Medicine, 1951.
Biskind, Morton S. Testimony before the House Select Committee to Investigate the Use of Chemicals in Food Products, 1950.
Scobey, Ralph R. Statement to the House Select Committee to Investigate the Use of Chemicals in Food Products, 1952.
Cholesterol and Heart Disease
Rokitansky, Karl von. A Manual of Pathological Anatomy. 1852.
Yerushalmy, J. and Hilleboe, H.E. “Fat in the Diet and Mortality from Heart Disease: A Methodologic Note.” New York State Journal of Medicine, 1957.
Kearns, C.E. et al. “Sugar Industry and Coronary Heart Disease Research: A Historical Analysis of Internal Industry Documents.” JAMA Internal Medicine, 2016.
McCully, Kilmer S. The Heart Revolution. HarperPerennial, 1999.
Rockefeller Medicine
Brown, E. Richard. Rockefeller Medicine Men: Medicine and Capitalism in America. University of California Press, 1979.
Flexner, Abraham. Medical Education in the United States and Canada (The Flexner Report). Carnegie Foundation, 1910.
Pharmaceutical Industry Influence
Gøtzsche, Peter C. Deadly Medicines and Organised Crime: How Big Pharma Has Corrupted Healthcare. Radcliffe Publishing, 2013.
Angell, Marcia. The Truth About the Drug Companies: How They Deceive Us and What to Do About It. Random House, 2004.
Light, Donald W. “Institutional Corruption of Pharmaceuticals and the Myth of Safe and Effective Drugs.” Journal of Law, Medicine & Ethics, 2013.
Virology
Bailey, Mark. A Farewell to Virology. 2022.
Epistemic Capture and the Streetlight Effect
Duke, Peter. Work on epistemic warfare and the architecture of manufactured ignorance.
Rogers, Toby. Testimony before the U.S. Senate on epistemic capture, 2025.
Unbekoming. “The Mechanics of Stable Falsehood.” Lies are Unbekoming, December 2025.
Unbekoming. “Epistemic Capture.” Lies are Unbekoming, September 2025.
Unbekoming. “The HPV Lie: Pap Smears, Gardasil, and a Cancer Caused by Something Else.” Lies are Unbekoming, January 2026.
Unbekoming. “Toxicology vs Virology: The Rockefeller Institute and the Criminal Polio Fraud.” Lies are Unbekoming, March 2025.
Unbekoming. “A Farewell to Virology (Expert Edition).” Lies are Unbekoming, January 2025.
Unbekoming. “The War on Knowing.” Lies are Unbekoming.
Unbekoming. “Extraction: The Middle Class as Colony.” Lies are Unbekoming, November 2025.
Unbekoming. “LeBron’s Immunity.” Lies are Unbekoming, December 2025.
Unbekoming. “The Wrong Enemy: Blood Clots. Not Cholesterol.” Lies are Unbekoming, September 2025.
January 31, 2026 Posted by aletho | Deception, Science and Pseudo-Science, Timeless or most popular | HPV vaccine, SSRIs, Statins | Leave a comment
The Weaponisation of Science
By Maryanne Demasi, PhD | October 22, 2025
Yesterday, I took part in a panel discussion in Washington, D.C., on the weaponisation of science — specifically, how conflicts of interest, industry influence, and scientific deception have reshaped modern medicine.
It was an important conversation about how the scientific process has been hollowed out by financial incentives, regulatory capture, and institutional cowardice.
For me, this is not an abstract debate. I’ve spent much of my career investigating how science becomes distorted — not by a few rogue actors, but through an entire system built on commercial dependence.
Once you start pulling the threads of how evidence is produced, who funds it, who controls the data, and who polices the outcomes, you quickly realise that the corruption of science is structural and systemic.
The Statin Wars: a case study in deception
I first saw this clearly while investigating cholesterol-lowering drugs. My 2013 Catalyst documentary questioned whether statins were being overprescribed, and it unleashed a media firestorm.
The episode was pulled after industry outrage, and I was publicly attacked. None of the critics engaged with the evidence — they simply sought to silence it.
In 2018, I published a narrative review, “Statin wars: have we been misled by the evidence?”
The piece revealed that the raw data underpinning statin trials were held exclusively by the Oxford-based Cholesterol Treatment Trialists (CTT) Collaboration and had never been released.
The CTT group had signed confidentiality agreements with pharmaceutical sponsors, blocking independent access to the raw data and preventing verification.
Yet those same meta-analyses have shaped prescribing guidelines around the world — produced by a group that sits under Oxford’s Clinical Trial Service Unit, which receives millions in funding from statin manufacturers.
In my public talks, I’ve described the statin story as a case study in bias and censorship. The trials used well-worn techniques to amplify benefits and minimise harms.
For example, they use ‘run-in’ periods before the trial to weed out people who couldn’t tolerate the drug, thereby artificially lowering the adverse events detected during the trial.
Often the outcomes were reported in relative, not absolute, terms — effectively exaggerating benefits that were, in reality, minuscule to the individual patient.
The vast majority of statin trials are funded by the manufacturers, and almost all show benefit — except for one publicly funded study that showed the opposite.
So, who funds the trial matters. The system is captured, plain and simple.
Regulatory capture and the illusion of oversight
The same dynamics pervade drug regulation. In a 2022 BMJ investigation, I showed how drug regulators rely heavily on funding from the very industries they oversee.
In Australia, the Therapeutic Goods Administration derives 96% of its operating budget from industry fees.
In the U.S., the same conflict exists through the Prescription Drug User Fee Act (PDUFA), which allows the FDA to collect billions from drug companies.
Those “user fees” now fund roughly two-thirds of the agency’s drug-review budget — a structural conflict of interest described by one scholar as “institutional corruption.”
And it’s true.
Industry money drives the demand for faster approvals through “expedited pathways,” which often means weaker evidence, shorter trials, and looser post‑marketing obligations.
Regulators defend this as “innovation,” yet the drugs approved under these pathways are far more likely to later receive black-box warnings or be withdrawn from the market due to safety issues.
The result is a system that rewards speed and sales over safety and substance.
The illusion of effective drugs has become even clearer thanks to a landmark investigation this year by Jeanne Lenzer and Shannon Brownlee.
They reviewed more than 400 FDA drug approvals between 2013 and 2022, and found that 73% of the drugs failed to meet four basic scientific criteria for demonstrating effectiveness.
Cancer drugs were especially problematic: only 3 out of 123 met all scientific standards, most approved on surrogate endpoints with no evidence they improved survival.
It’s the perfect illustration of regulatory capture — an agency funded by industry fees and pressured by politics, approving drugs of uncertain benefit while calling itself the “gold standard.”
Antidepressant deception
The same playbook has unfolded in psychiatry — beginning with how clinical trials are designed and reported.
Study 329 is one of the best-known examples. It claimed that paroxetine (Paxil) was safe and effective for adolescents aged 12 to 18.
But when researchers reanalysed the original regulatory documents, they found that suicides and suicide attempts had been coded under misleading terms such as “emotional lability” or “worsening depression,” effectively erasing them from view.
A similar pattern emerged when regulatory documents for two fluoxetine (Prozac) trials in children and adolescents were re-examined. Suicide attempts were omitted or misclassified, making the drug appear safer than it was.
Both reanalyses were carried out under the Restoring Invisible and Abandoned Trials (RIAT) initiative, a project dedicated to “restoring” abandoned or misreported trials by publishing accurate versions of the data submitted to regulators.
Selective publication compounds the problem.
The FDA only requires two trials demonstrating a drug is better than placebo before it is approved – meaning multiple failed trials get buried.
Psychologist Irving Kirsch, using Freedom of Information requests, uncovered dozens of unpublished SSRI trials that had been withheld from the medical literature.
When those missing studies were included, the apparent benefit of antidepressants over placebo almost vanished — an average gain of less than two points on the Hamilton Depression Scale, far below the threshold for meaningful clinical benefit.
In other words, much of what appears to be a “drug effect” is, in reality, placebo.
For years, patients have also been sold the marketing myth that depression stems from a “chemical imbalance” in the brain — a debunked theory but an extraordinarily effective sales campaign.
In 2020, we analysed popular health websites across ten countries and found that about 74% falsely claimed depression was caused by a chemical imbalance and implied that antidepressants could correct it.
It may sound like harmless messaging, but its influence is profound.
An Australian study showed that 83% of people who were told they had a chemical imbalance were more likely to take an antidepressant, believing it would “fix” their brain chemistry.
A more recent review in Molecular Psychiatry synthesised the best available evidence and found no consistent link between depression and low serotonin levels or activity.
Together, these findings reveal how psychiatry’s modern narrative was constructed — through distorted trials and deceptive marketing — turning uncertainty into certainty, and speculation into “science.”
Fraud by omission
Recently, I reported on how journals can weaponise science.
The BMJ’s Peter Doshi raised serious concerns about the pivotal PLATO trial for the anti-clotting drug ticagrelor — including data irregularities and unexplained deaths. But the journal Circulation that published the trial, has refused to investigate.
This selective vigilance is telling. Journals will retract small hypothesis papers that challenge orthodoxy, but billion‑dollar drugs with questionable data remain untouchable.
We’ve seen an even more aggressive form of suppression in the vaccine arena.
The recent Covaxin case exposed the extent to which manufacturers will go to suppress inconvenient findings.
After Indian researchers published a peer‑reviewed post‑marketing study suggesting serious adverse events “might not be uncommon,” Bharat Biotech — the vaccine’s manufacturer — filed a defamation lawsuit against the 11 authors and the journal’s editor, demanding retraction and millions in damages.
Within weeks, the journal caved, announcing its intention to retract despite finding no scientific fraud or fabrication. The only “offence” was to suggest that further safety research was warranted.
It’s a chilling example of how corporate and political power now overrides the normal mechanisms of scientific debate — a new form of censorship disguised as quality control.
Punishing scientists
The weaponisation of science isn’t only about suppressing inconvenient ideas or studies—it extends to the scientists themselves.
During the Vioxx scandal, Merck was caught keeping an actual “hit list” of doctors and academics who criticised the drug’s cardiovascular risks.
Internal emails revealed executives discussing plans to “seek them out and destroy them where they live.” That’s how far industry will go to silence dissent.
Executives are no longer stupid enough to put such threats in writing, but the behaviour persists — now outsourced to lobby groups and front organisations that quietly destroy reputations.
I experienced a version of this myself after my ABC documentaries on statins and sugar.
Like Merck, the Australian Breakfast Cereal Manufacturers Forum – an industry front group – drew up an “active defence” plan to neutralise me for challenging the industry narrative.
And we’ve seen it again recently with the leaked BIO memo detailing a coordinated plan to undermine Health Secretary Robert F. Kennedy Jr. — by co-opting media influencers, partnering with think tanks, and shaping public perception.
Different industries, same playbook: when billions are at stake, dissent is dangerous, and science becomes a weapon.
Weaponised fact-checkers
Look at the rise of fact-checking as a weapon.
In 2024, for example, a peer‑reviewed Japanese study published in the journal Cureus that reported a statistical rise in certain cancers following the Covid‑19 mRNA vaccine rollout was retracted after a Reuters “fact check.”
The authors, led by Dr Miki Gibo, made no claim of causation and had explicitly called for further investigation, yet the journal retracted the paper after the media controversy, citing concerns about the scrutiny of fact checkers.
When journals begin outsourcing editorial judgment to media organisations with commercial or institutional conflicts, peer review itself collapses under the weight of narrative control.
This is what I mean by the weaponisation of science.
Fraud today isn’t only about fabricating data — it’s about what institutions choose to suppress. It’s selective enforcement designed to protect profits under the guise of integrity.
Can we restore scientific honesty?
I’m not going to pretend I have all the answers. Whether it’s cholesterol or serotonin, the science too often bends toward profit rather than truth.
Regulators, journals, and academic institutions have become so financially entangled with industry that truly independent science is now the exception, not the rule.
Retractions, fact-checks, and editorial bans are deployed selectively — not to correct fraud, but to erase debate under the banner of “scientific consensus.”
We’ve tried to fix this with transparency measures like open-data policies and the Sunshine Act, which expose payments from pharmaceutical companies to doctors.
But disclosure has become a box-ticking exercise and raw data is still hard to get. Meanwhile, the machinery of influence keeps turning.
The deeper problem is the absence of accountability. Without accountability, there can be no trust.
When Merck’s painkiller Vioxx was withdrawn after being linked to tens of thousands of deaths, not one executive went to jail. The company paid fines, issued statements, and carried on.
Lives were lost, and no one was held personally responsible. That isn’t justice — it’s the “cost of doing business,” and worse, the people who preside over these disasters are often rewarded for them.
Bonuses are paid, stock options soar, and departing CEOs collect multimillion-dollar severance packages — all while families are left to bury their dead.
If we’re serious about restoring trust, that has to change. CEOs and senior executives who knowingly conceal data or market dangerous drugs should face criminal penalties, not corporate settlements.
A few jail sentences at the top would do more to restore trust in medicine than a thousand press releases about a renewed commitment to safety.
Accountability must also extend to government.
The FDA and other regulators are structurally dependent on industry money. It’s baked into the system, and the only real solution is to rebuild — fund these agencies publicly, remove user fees, and make them independent again.
The barrier isn’t money — it’s political will, compromised by the same corporate lobbying and campaign donations that distort science.
True reform requires the courage to confront the pharmaceutical industry’s financial grip on both major parties, to end the political donations that buy silence, and to legislate for genuine independence in science and medicine.
Perhaps Secretary Kennedy is now best placed to begin dismantling industry’s hold on science. Systemic corruption didn’t happen overnight, and it won’t be undone overnight either.
Commercial conflicts of interest have become normalised — woven through our institutions, universities, journals, and political culture. Until that’s confronted directly, nothing will change.
Disclosure is necessary, but it is not sufficient. The antidote is open debate, public funding, and real accountability.
Science should never be about consensus; it should be about contestability. If we can’t test claims, challenge data, or ask uncomfortable questions without fear of retribution, then we no longer have science — we have marketing.
The weaponisation of science ends only when truth becomes more valuable than profit.
October 23, 2025 Posted by aletho | Corruption, Deception, Science and Pseudo-Science, Timeless or most popular | Statins | Leave a comment
How You’ve Been Misled About Statins
By Dr. Joseph Mercola | March 11, 2020
Statins are HMG-CoA reductase inhibitors; that is, they block the enzyme in your liver responsible for making cholesterol (HMG-CoA reductase). According to Drugs.com, more than 35 million Americans are on a statin drug, making it one of the most commonly prescribed medicines in the U.S.1
National Health and Nutrition Examination Survey data suggest 47.6% of seniors over the age of 75 are on a statin drug.2 Lipitor — which is just one of several brand name statin drugs — is one of the most profitable drugs in the history of medicine.3,4
Collectively, statins have earned over $1 trillion since they were introduced.5 This, despite their being off patent. There is simply no doubt that selling them is big business with major financial incentives to distort the truth to continue their sales.
Statin recommendations have become fairly complex, as they’re recommended for various age groups under different circumstances, and whether they’re used as primary prevention of cardiovascular disease (CVD), or secondary prevention. Guidelines also vary slightly depending on the organization providing the recommendation and the country you’re in.6
In the U.S., the two guidelines available are from the U.S. Preventive Services Task Force (USPSTF),7 and the American College of Cardiology and American Heart Association.8,9 The USPSTF guidelines recommend using a statin for the primary prevention of CVD when a patient:10
- Is between the age of 40 to 75
- Has one or more CVD risk factors (dyslipidemia, diabetes, hypertension or smoking)
- Has a calculated 10-year risk of a cardiovascular event of 10% or greater
In secondary prevention of CVD, statins are “a mainstay,” according to the Journal of the American College of Cardiology.11 Secondary prevention means the drug is used to prevent a recurrence of a heart attack or stroke in patients who have already had one.
Regulators’ Role Questioned
A February 2020 analysis12 in BMJ Evidence-Based Medicine (paywall) brings up the fact that while the use of statins in primary prevention of CVD “has been controversial” and there’s ongoing debate as to “whether the benefits outweigh the harms,” drug regulators around the world — which have approved statins for the prevention of CVD — have stayed out of the debate. Should they? The analysis goes on to note:
“Our aim was to navigate the decision-making processes of European drug regulators and ultimately request the data upon which statins were approved. Our findings revealed a system of fragmented regulation in which many countries licensed statins but did not analyze the data themselves.
There is no easily accessible archive containing information about the licensing approval of statins or a central location for holding the trial data. This is an unsustainable model and serves neither the general public, nor researchers.”
Have We Been Misled by the Evidence?
In her 2018 peer-reviewed narrative review,13 “Statin Wars: Have We Been Misled About the Evidence?” published in the British Journal of Sports Medicine, Maryanne Demasi, Ph.D., a former medical science major turned investigative health reporter, delves into some of these ongoing controversies.
“A bitter dispute has erupted among doctors over suggestions that statins should be prescribed to millions of healthy people at low risk of heart disease. There are concerns that the benefits have been exaggerated and the risks have been underplayed.
Also, the raw data on the efficacy and safety of statins are being kept secret and have not been subjected to scrutiny by other scientists. This lack of transparency has led to an erosion of public confidence.
Doctors and patients are being misled about the true benefits and harms of statins, and it is now a matter of urgency that the raw data from the clinical trials are released,” Demasi writes.14
While Demasi’s paper is behind a paywall, she reviews her arguments in the featured video above. Among them is the fact that the “statin empire” is built on prescribing these drugs to people who really don’t need them and are likely to suffer side effects without getting any benefits.
For example, some have recommended statins should be given to everyone over the age of 50, regardless of their cholesterol level. Others have suggested screening and dosing young children.
Even more outrageous suggestions over the past few years include statin “‘condiments’ in burger outlets to counter the negative effects of a fast food meal,'” and adding statins to the municipal water supply.
Simple Tricks, Big Payoffs
Medical professionals are now largely divided into two camps, one saying statins are lifesaving and safe enough for everyone, and the other saying they’re largely unnecessary and harmful to boot. How did such a divide arise, when all have access to the same research and data?
Demasi suggests that in order to understand how health professionals can be so divided on this issue, you have to follow the money. The cost of developing and getting market approval for a new drug exceeds $2.5 billion. “A more effective way to fast-track company profits is to broaden the use of an existing drug,” Demasi says, and this is precisely what happened with statins.
By simply revising the definition of “high cholesterol,” which was done in 2000 and again in 2004, millions of people became eligible for statin treatment, without any evidence whatsoever that it would actually benefit them.
As it turns out, eight of the nine members on the U.S. National Cholesterol Education Program panel responsible for these revisions had “direct ties to statin manufacturers,” Demasi says, and that public revelation sowed the first seed of suspicion in many people’s minds.
Skepticism ratcheted up even more when, in 2013, the American College of Cardiology and AHA revised their statin guideline to include a CVD risk calculation rather than a single cholesterol number. U.S. patients with a 7.5% risk of developing CVD in the next 10 years were now put on a statin. (In the U.K., the percentage used was a more reasonable 20%.)
This resulted in another 12.8 million Americans being put on statin treatment even though they didn’t have any real risk factors for CVD. Worse, a majority of these were older people without heart disease — the very population that stand to gain the least from these medications.
What’s worse, 4 of 5 calculators were eventually found to overestimate the risk of CVD, some by as much as 115%, which means the rate of overprescription was even greater than previously suspected.
Industry Bias
While simple revisions of the definitions of high cholesterol and CVD risk massively augmented the statin market, industry-funded studies have further fueled the overprescription trend. As noted by Demasi, when U.S. President Ronald Reagan cut funding to the National Institutes of Health, private industry moved in to sponsor their own clinical trials.
The vast majority of statin trials are funded by the manufacturers, and research has repeatedly found that funding plays a major role in research outcomes. It’s not surprising then that most statin studies overestimate drug benefits and underestimate risks.
Demasi quotes Dr. Peter Gøtzsche, a Danish physician-researcher who in 1993 co-founded the Cochrane Collaboration and later launched the Nordic Cochrane Centre:
“When drug industry sponsored trials cannot be examined and questioned by independent researchers, science ceases to exist and it becomes nothing more than marketing.”
“The very nature of science is its contestability,” Demasi notes. “We need to be able to challenge and rechallenge scientific results to ensure they’re reproducible and legitimate.” However, there’s been a “cloud of secrecy” around clinical statin trials, Demasi says, as the raw data on side effects have never been released to the public, nor other scientists.
The data are being held by the Cholesterol Treatment Trialists (CTT) Collaboration at CTSU Oxford, headed by Rory Collins, which periodically publishes meta-analyses of the otherwise inaccessible data. While the CTT claims to be an independent organization, it has received more than £260 million from statin makers.
Inevitably, its conclusions end up promoting wider use of statins, and no independent review is possible to contest or confirm the CTT Collaboration’s conclusions.
Tricks Used to Minimize Harms in Clinical Trials
As explained by Demasi, there are many ways in which researchers can influence the outcome of a drug trial. One is by designing the study in such a way that it minimizes the chances of finding harm. The example she gives in her lecture is the Heart Protection Study.
Before the trial got started, all participants were given a statin drug for six weeks. By the end of that run-in period, 36% of the participants had dropped out due to side effects or lack of compliance. Once they had this “freshly culled” population, where those suffering side effects had already been eliminated, that’s when the trial actually started.
Now, patients were divided into statin and placebo groups. But since everyone had already taken a statin before the trial began, the side effects found in the statin and placebo groups by the end of the trial were relatively similar.
In short, this strategy grossly underestimates the percentage of the population that will experience side effects, and this “may explain why the rate of side effects in statin trials is wildly different from the rate of side effects seen in real-world observations,” Demasi says.
Deception Through Statistics
Public opinion can also be influenced by exaggerating statistics. A common statistic used to promote statins is that they lower your risk of heart attack by about 36%.15 This statistic is derived from a 2008 study16 in the European Heart Journal. One of the authors on this study is Rory Collins, who heads up the CTT Collaboration.
Table 4 in this study shows the rate of heart attack in the placebo group was 3.1% while the statin group’s rate was 2% — a 36% reduction in relative risk. However, the absolute risk reduction — the actual difference between the two groups, i.e., 3.1% minus 2% — is only 1.1%, which really isn’t very impressive.
In other words, in the real world, if you take a statin, your chance of a heart attack is only 1.1% lower than if you’re not taking it. At the end of the day, what really matters is what your risk of death is the absolute risk. The study, however, only stresses the relative risk (36%), not the absolute risk (1.1%).
As noted in the review,17 “How Statistical Deception Created the Appearance That Statins Are Safe and Effective in Primary and Secondary Prevention of Cardiovascular Disease,” it’s very easy to confuse and mislead people with relative risks. You can learn more about absolute and relative risk in my 2015 interview with David Diamond, Ph.D., who co-wrote that paper.
Silencing Dissenters and Fear-Based PR
Yet another strategy used to mislead people is to create the illusion of “consensus” by silencing dissenters, discrediting critics and/or censoring differing views.
In her lecture, Demasi quotes Collins of the CTT Collaboration saying that “those who questioned statin side effects were ‘far worse’ and had probably ‘killed more people’ than ‘the paper on the MMR vaccine'” … “Accusing you of murdering people is an effective way [to] discredit you,” she says.
Demasi also highlights the case of a French cardiologist who questioned the value of statins in his book. It received widespread attention in the French press, until critics started saying the book and resulting press coverage posed a danger to public health.
One report blamed the book for causing a 50% increase in statin discontinuation, which was predicted would lead to the death of 10,000 people. On this particular occasion, however, researchers analyzed the number of actual deaths based on national statistics, and found the actual death toll decreased in the year following the release of the book.
The authors, Demasi says, noted that it was “‘not evidence-based to claim that statin discontinuation increases mortality,’ and that in the future, scientists should assess ‘real effects of statin discontinuation rather than making dubious extrapolations and calculations.'”
Trillion-Dollar Business Based on Flimsy Evidence
Statins, originally introduced three decades ago as secondary prevention for those with established CVD and patients with congenital and familial hyperlipidemias, have now vastly expanded thanks to the strategies summarized above.
Tens if not hundreds of millions of people are now on these drugs, without any scientific evidence to show they will actually benefit from them. As noted in the EBM analysis, “Statins for Primary Prevention: What Is the Regulator’s Role?”:18
“The central clinical controversy has been a fierce debate over whether their benefits in primary prevention outweigh their harms … The largest known statin usage survey conducted in the USA found that 75% of new statin users discontinued their therapy by the end of the first year, with 62% of them saying it was because of the side effects.
Regardless of what level of prevention statin prescription is aimed at, the proposed widening of the population to over 75s de facto includes people with multiple pathologies, whether symptomatic or not, and bypasses the distinction between primary and secondary prevention …
The CTT Collaboration estimates the frequency of myopathy is quite rare, at five cases per 10,000 statin users over five years. But others have contended that the CTT Collaboration’s work ‘simply does not match clinical experience’ … [Muscle-related adverse events] reportedly occur with a frequency of … as many as 20% of patients in clinical practice.”
Regulators Have a Duty to Create Transparency
Considering the discrepancy in reported side effects between statin trials, clinical practice and statin usage surveys, what responsibility do regulators have?
According to “Statins for Primary Prevention: What Is the Regulator’s Role?”19 regulators have a responsibility to “engage and publicly articulate their position on the controversy and make the evidence base underlying those judgments available to third parties for independent scrutiny,” none of which has been done to date. The paper adds:
“Regulators holding clinical trial data, particularly for public health drugs, should make these data available in searchable format with curated and dedicated web-based resource. If national regulators are not resourced for this, pooling or centralizing resources may be necessary.
The isolation of regulators from the realities of prescribing medications based on incomplete or distorted information is not enshrined in law but is a product of a subculture in which commercial confidentiality is more important than people. This also needs to change.”
Do Your Homework Before Taking a Statin
There’s a lot of evidence to suggest drug company-sponsored statin research and its PR cannot be trusted, and that few of the millions of people currently taking these drugs actually benefit from them.
Some of the research questioning the veracity of oft-cited statin trials is reviewed in “Statins’ Flawed Studies and Flawed Advertising” and “Statins Shown to Extend Life by Mere Days.”
To learn more about the potential harms of statins, see “Statins Double Diabetes Rates,” “Statins Trigger Brain Changes With Devastating Effects,” and “5 Great Reasons You Should Not Take Statins.”
Sources and References
- 1 Drugs.com September 10, 2018
- 2 AAFP.org, Statin Use for Primary Prevention of CVD in Adults
- 3 Youtube.com Maryanne Demasi, Statin Wars: Have We Been Misled by the Evidence?, 1:40 minutes
- 4 Kiplinger December 1, 2017
- 5 BMJ January 21, 2018
- 6 American College of Cardiology, Statin Use in Primary Prevention of ASCVD According to 5 Guidelines
- 7, 10 AAFP.org, Statin Use for Primary Prevention of CVD in Adults: Recommendation Statement
- 8 2019 American College of Cardiology and American Heart Association Guideline on the Primary Prevention of Cardiovascular Disease
- 9 Mayo Clinic Cholesterol Guidelines
- 11 Journal of the American College of Cardiology June 2017; 69(22)
- 12 BMJ Evidence-Based Medicine 26 February 2020 [Epub ahead of print] DOI: 10.1136/bmjebm-2019-111321
- 13, 14 British Journal of Sports Medicine 2018;52:905-909
- 15 Youtube.com Maryanne Demasi, Statin Wars: Have We Been Misled by the Evidence?, 14:40 minutes
- 16 European Heart Journal February 1, 2008; 29(4): 499-508
- 17 Expert Review of Clinical Pharmacology March 2015:8(2); 201-210
- 18, 19 BMJ Evidence-Based Medicine 26 February 2020 [Epub ahead of print] DOI: 10.1136/bmjebm-2019-111321, Introduction
January 25, 2022 Posted by aletho | Science and Pseudo-Science, Timeless or most popular, Video | Statins | Leave a comment
Statins Do More Harm Than Good
By Dr. Joseph Mercola | January 15, 2022
Amid the pandemic media storm in January 2021, a study1 published in the journal Atherosclerosis quietly revealed that people taking statin medications had a higher rate of cardiovascular events than those who were not on statins.2
In the study, the researchers separated the participants by assigning them a coronary artery calcium (CAC) score. This is a noninvasive CT scan designed to detect plaque buildup in your coronary arteries. It is also called a cardiac calcium score,3 calcium scan or Agatston score.4
Doctors use this score to calculate your risk of developing coronary artery disease as it measures calcified plaque within the arteries. Data has shown your risk of heart disease correlates with this score. The lower the score, the less likely you are to have a cardiac event when compared against other men and women your age. The score ranges from zero to over 400.5
- Zero — No plaque with a low risk of a heart attack.
- 1-10 — Small amount of plaque and less than 10% chance of heart disease.
- 11-100 — Some plaque with mild heart disease and a moderate risk of a heart attack.
- 101-400 — Moderate amount of plaque that may block a coronary artery, with a moderate to high risk of a heart attack.
- 400+ — Large amount of calcified plaque is found in the coronary arteries with more than a 90% chance it is blocking an artery.
Doctors consider a CAC test if you are between 40 and 70 with an increased risk for heart disease but do not have symptoms.6 People with a family history of heart disease, who are a past or present smoker, are overweight, are inactive or have a history of high cholesterol, diabetes or high blood pressure have factors that increase their risk of heart disease.
Yet, not all physicians use the CAC score as recommended. Writing for the Texas Heart Institute, the assistant medical director, Dr. Stephanie Coulter, says, “When my high-risk patients are not taking their cholesterol-lowering statin medicine, the calcium score can be a very powerful motivator for them to follow my professional advice and prescription.”7
However, further into her article, she stresses the test is only appropriate for moderate-risk patients, and those with a low or high risk of heart disease do not benefit from the scan. The study published in Atherosclerosis indicates that even with a high CAC score, taking statins does not reduce your risk of a cardiovascular event and may, in fact, increase it.8,9
Data Show Statins Increase Your Risk for Heart Events
The researchers were working under the premise that statins do not decrease the CAC score and may increase calcification.10 They used the prognostic significance of CAC when compared against statin users in 28,025 patients ages 40 to 75 years. The researchers adjusted the data for traditional cardiovascular disease risk factors and examined the performance of CAC volume, density and area.
Nearly 11 months after the results were published, Tucker Goodrich11 extracted the data from Table 1 into a graphic representation that demonstrated only in the highest CAC score range of 400 or greater were the data nearly identical between those taking statins and those not taking statins. Otherwise, those taking statins always had more cardiac events than those who weren’t. The researchers concluded that:12
“CAC scoring retains robust risk prediction in statin users, and the changing relationship of CAC density with outcomes may explain the slightly weaker relationship of CAC with outcomes in statin users.”
The researchers acknowledged that true to the recommended use of CAC scoring, only a baseline score was known, so they were unable to evaluate whether statins influenced the progression of calcification. There was limited race and ethnic diversity within the study group.
Yet, despite the limitations of the design and the results, they believe the analysis used data from one of the largest samples available to date and provides “both real-world and investigational support for the role of CAC in risk stratifying patients taking statins.”13
Tucker Goodrich14 quotes from an article in the American College of Cardiology published January 2021, in which the writers analyzed the data. They wrote:15
“The findings confirm that CAC does have prognostic value among statin users, although the association is attenuated. Complicating interpretation is the inclusion of only fatal events and the relatively elevated, but still low, mortality rate in statin users versus non-users with a zero CAC score.
A key mechanism underlying this phenomenon is that statins increase plaque density thereby paradoxically raising the Agatston CAC score — as density is upweighted.”
There appears to be some discrepancy. First, the data that show people with a CAC score of zero — no plaque and low risk — were inexplicably taking statins. Secondly, the study acknowledges that there was one baseline CAC score taken, so how much the plaque density increased or didn’t increase in this population could not be ascertained.
And finally, the raw data showed people on statins died more frequently than those who didn’t take the drug in nearly every CAC category. However, the writers postulated that the increasing plaque density that raises the CAC score may be overcome by expanding the scoring method and investigating the protective role that densely calcified plaque may play in cardiovascular health:16
“However, this is hampered by a current lack of reference values, limited supportive research, and validation; implementation limitations include software update requirements and standardization.”
In other words, expanding the CAC scoring, which should be taken before prescribing statins and is not recommended as a follow-up since it exposes patients to the same radiation as 10 X-rays,17 may possibly alter the results enough that it reflects greater benefit to using statins.
Statins Are More Than a Colossal Waste of Money
Despite decades of statin drug use and vilification of saturated fats and cholesterol, heart disease remains the No. 1 cause of death.18 Although the researchers in the featured study do not mention it, their data support past research that shows statins are a colossal waste of money, and likely more.
In 2014, Maryanne Demasi, Ph.D., produced a documentary, “Heart of The Matter: Dietary Villains.” The film exposed the myths behind the statin fad and the financial links that drove the industry. It was so thorough that vested interests convinced ABC-TV to rescind the two-part series and got the documentary expunged.19
Since the release of that documentary, the evidence against the cholesterol theory and statins has only grown. Dr. Malcolm Kendrick, a general practitioner with the British National Health Service, expressed his disbelief at how widely statins are used despite research evidence they are not effective, and possibly worse. He wrote:20
“New research shows that the most widely prescribed type of drug in the history of medicine is a waste of money. One major study found that the more ‘bad’ cholesterol was lowered, the greater the risk of heart attacks and strokes.
In the midst of the COVID-19 pandemic, almost every other medical condition has been shoved onto the sidelines. However, in the UK last year, heart attacks and strokes (CVD) killed well over 100,000 people — which is at least twice as many as have died from COVID-19.
CVD will kill just as many this year, which makes it significantly more important than COVID-19, even if no one is paying much attention to it right now.”
What data have demonstrated is that statin medications are not inert, and in fact can damage your health while not protecting your heart. One of the side effects of lower cholesterol levels is impaired cognitive performance.21
One study22 showed patients with mild cognitive impairment had double the risk of dementia when using lipophilic statins, such as atorvastatin (Lipitor), simvastatin (Zocor), Fluvastatin (Lescol), and lovastatin (Altoprev), which dissolve more readily in fats.23
This Harvard article claims those same drugs that increase the risk of dementia may lower your risk of liver cancer, which is not a choice any patient should have to make. There is also evidence to suggest people taking statins have twice the risk of being diagnosed with diabetes than those who do not and taking the drug for longer than two years triples the risk. One of the scientists from The Ohio State University explained in a press release:24
“The fact that increased duration of statin use was associated with an increased risk of diabetes — something we call a dose-dependent relationship — makes us think that this is likely a causal relationship.”
Not all data show that people taking statins have more heart events than people not taking statins. Some, like this systematic review25 published in 2015, found that despite the added risks of dementia and diabetes, people taking statins could live an average of only 3.2 to 4.1 days longer than if they didn’t take the drug.
Your Body Requires Cholesterol to Live
The triggers for cardiovascular disease are more complex than just lowering cholesterol levels. As data have shown us, lowering cholesterol is not the panacea for avoiding heart disease and extending your life. Kendrick refutes the idea that the LDL-cholesterol hypothesis is accurate, writing:26
“For the LDL hypothesis to be correct, it requires that LDL can travel past the lining of the artery, the endothelial cells, and into the artery wall behind. This is considered the starting point for atherosclerotic plaques to form. The problem with this hypothesis is that LDL cannot get into any cell, let alone an endothelial cell, unless that cell wants it to.”
However, damage to the arterial walls can be induced by several factors, including high blood pressure, inflammation, elevated blood sugar and smoking.27 Once damaged, plaque begins to build up as a protective mechanism. The problem arises when the rate of damage and result in clot formation outpace your body’s ability to repair it.
Instead, it’s crucial that you understand how important cholesterol is to the human body. In fact, according to Zoe Harcombe, Ph.D., nutritional researcher, author and public speaker, “If you had no cholesterol in your body, you would be dead.”28
As noted by Harcombe, the notion that there is good and bad cholesterol is also wrong. LDL and high-density lipoprotein (HDL) are not even cholesterol but, rather, carriers and transporters of cholesterol, triglycerides (fat), phospholipids and proteins. “LDL would more accurately be called the carrier of fresh cholesterol and HDL would more accurately be called the carrier of recycled cholesterol,” she says.29
How to Identify and Lower Your Risk for Heart Disease
Using simple strategies at home may help normalize your cholesterol and blood sugar levels. I believe a total cholesterol measurement has little benefit in evaluating your risk for heart disease unless the total number is over 300.
In some instances, high cholesterol may indicate a problem when your LDL or triglycerides are high, and your HDL is low. You’ll be better able to evaluate your risk by looking at the two ratios below, in combination with other lifestyle factors such as ferritin and gamma-glutamyl transpeptidase (GGT) tests. To calculate your cholesterol ratios:30,31,32
- Cholesterol:HDL ratio — Divide your total cholesterol by your HDL level. Ideally, the ratio should be below 5-to1; a ratio below 3.5-to1 is considered optimal
- Triglyceride:HDL ratio — Divide your triglyceride level by your HDL. This ratio should ideally be below 2
However, rather than focusing on cholesterol, there are two tests far more important for assessing your CVD risk. These are the serum ferritin33 and gamma-glutamyl transpeptidase (GGT) tests.34 The GGT test can be used as a screening marker for excess free iron and is a great indicator of your sudden cardiac death risk.
To protect yourself against heart disease, here are several suggestions that help lower your insulin resistance and restore insulin sensitivity, among other heart-protective mechanisms:
- Avoid environmental pollutants and toxins, including smoking, vaping, heavy metals, herbicides and pesticides, especially glyphosate.
- Minimize your exposure to electromagnetic fields and wireless radiation from cellphones, Wi-Fi, routers, smart meters and more, as this kind of radiation has been shown to cause serious free radical damage and mitochondrial dysfunction.
- Eat an unprocessed whole food-based diet low in net carbs and high in healthy fats. A ketogenic diet — which is very low in net carbohydrates and high in healthy fats — is key for boosting mitochondrial function.
- When your body can burn fat for fuel, your liver creates water-soluble fats called ketones that burn far more efficiently than carbs, thereby creating fewer reactive oxygen species and secondary free radicals. Ketones also decrease inflammation and improve glucose metabolism.35
- Eat nitrate-rich foods to help normalize your blood pressure. Good sources include arugula, cilantro, rhubarb, butter leaf lettuce, mesclun mixed greens, beet greens, fresh beet juice, kvass (fermented beet juice) and fermented beet powder.
- Get plenty of non-exercise movement each day; walk more and incorporate higher intensity exercise as your health allows.
- Intermittently fast. After you’ve become accustomed to intermittently fasting for 16 to 18 hours, you can try a stricter fast once or twice a week, when you eat a 300- to 800-calorie meal loaded with detox-supporting nutrients, followed by a 24-hour fast. So, in essence, you’re then only eating one 300- to 800-calorie meal in 42 hours.
- If you have heart disease, consider enhanced external counterpulsation (EECP). To find a provider, see EECP.com.36
- Get sensible sun exposure to optimize your vitamin D status and/or take an oral vitamin D3 supplement with magnesium and vitamin K2.
- Implement heart-based wellness practices such as connecting with loved ones and practicing gratitude.
Sources and References
- 1, 8 Atherosclerosis, 2021;316
- 2, 9, 11 Twitter, Tucker Goodrich, December 23, 2021
- 3, 6 Cleveland Clinic, Calcium-Score Screening
- 4 University of Maryland Medical Center, Cardiac Calcium Scoring, About your CAC score
- 5 University of Maryland Medical Center, Cardiac Calcium Scoring, Calcium score results
- 7 Texas Heart Institute, Do I Need a Coronary Calcium Score?
- 10 Atherosclerosis, 2021;316 Abstract/Background/Aims
- 12 Atherosclerosis, 2021;316 Abstract/Concl
- 13 Atherosclerosis, 2021;316 Discussion last line
- 14 Twitter, Tucker Goodrich, December 23, 2021, 3 of 4
- 15, 16 American College of Cardiology, January 19, 2021
- 17 Texas Heart Institute, Do I Need a Coronary Calcium Score? Are there any risks to this procedure?
- 18 Centers for Disease Control and Prevention, Leading Causes of Death
- 19 Highstreaks May 21, 2014, Section – Update
- 20 RT, August 4, 2020
- 21 Frontiers in Neurology, doi.org/10.3389/fneur.2018.00952
- 22 Journal of Nuclear Medicine May 2021, 62
- 23 Harvard Health Publishing, January 27, 2020, 50% down the page, search on “lipitor”
- 24 The Ohio State University, June 25, 2019
- 25 BMJ Open 2015 Sep 24;5(9):e007118 Abstract/Results
- 26, 27 Dr. Malcolm Kendrick, November 27, 2018
- 28 ZoeHarcombe.com, We have got cholesterol completely wrong Point 1
- 29 ZoeHarcombe.com, We have got cholesterol completely wrong Point 3
- 30 Mayo Clinic
- 31 University of Rochester Medical Center
- 32 Journal-Advocate February 27, 2012
- 33 Int J Prev Med. 2013 Aug; 4(8): 911–916
- 34 Ann Transl Med. 2016 Dec; 4(24): 481
- 35 IUMB Life April 3, 2017, DOI: 10.1002/iub.1627
- 36 EECP.com
January 16, 2022 Posted by aletho | Science and Pseudo-Science, Timeless or most popular | Statins | Leave a comment
APOE-4: The Clue to Why Low Fat Diet and Statins may Cause Alzheimer’s
By Dr. Stephanie Seneff | December 15, 2009
Abstract
Alzheimer’s is a devastating disease whose incidence is clearly on the rise in America. Fortunately, a significant number of research dollars are currently being spent to try to understand what causes Alzheimer’s. ApoE-4, a particular allele of the apolipoprotein apoE, is a known risk factor. Since apoE plays a critical role in the transport of cholesterol and fats to the brain, it can be hypothesized that insufficient fat and cholesterol in the brain play a critical role in the disease process. In a remarkable recent study, it was found that Alzheimer’s patients have only 1/6 of the concentration of free fatty acids in the cerebrospinal fluid compared to individuals without Alzheimer’s. In parallel, it is becoming very clear that cholesterol is pervasive in the brain, and that it plays a critical role both in nerve transport in the synapse and in maintaining the health of the myelin sheath coating nerve fibers. An extremely high-fat (ketogenic) diet has been found to improve cognitive ability in Alzheimer’s patients. These and other observations described below lead me to conclude that both a low-fat diet and statin drug treatment increase susceptibility to Alzheimer’s.
1. Introduction
Alzheimer’s is a devastating disease that takes away the mind bit by bit over a period of decades. It begins as odd memory gaps but then steadily erodes your life to the point where around-the-clock care is the only option. With severe Alzheimer’s, you can easily wander off and get lost, and may not even recognize your own daughter. Alzheimer’s was a little known disease before 1960, but today it threatens to completely derail the health system in the United States.
Currently, over 5 million people in America have Alzheimer’s. On average, a person over 65 with Alzheimer’s costs three times as much for health care as one without Alzheimer’s. More alarmingly, the incidence of Alzheimer’s is on the rise. Dr. Murray Waldman has studied epidemiological data comparing Alzheimer’s with femur fractures, looking back over the last fifty years [52]. Alarmingly, he has found that, while the incidence of femur fractures (another condition which typically increases with age) has gone up only at a linear rate, the increase in the incidence of Alzheimer’s has gone up exponentially, between 1960 and 2010 Alzheimer’s Epidemic [15]. Just between 2000 and 2006, US Alzheimer’s deaths rose by 47%, while, by comparison, deaths from heart disease, breast cancer, prostate cancer, and stroke combined decreased by 11%. This increase goes far beyond people living longer: for people 85 and older, the percentage who died from Alzheimer’s rose by 30% between 2000 and 2005 [2]. Finally, it’s likely these are under-estimates, as many people suffering with Alzheimer’s ultimately die of something else. You likely have a close friend or relative who is suffering from Alzheimer’s.
Something in our current lifestyle is increasing the likelihood that we will succumb to Alzheimer’s. My belief is that two major contributors are our current obsession with low-fat diet, combined with the ever expanding use of statin drugs. I have argued elsewhere that low-fat diet may be a major factor in the alarming increase in autism and adhd in children. I have also argued that the obesity epidemic and the associated metabolic syndrome can be traced to excessive low-fat diet. Statins are likely contributing to an increase in many serious health issues besides Alzheimer’s, such as sepsis, heart failure, fetal damage, and cancer, as I have argued here. I believe the trends will only get worse in the future, unless we substantially alter our current view of “healthy living.”
The ideas developed in this essay are the result of extensive on-line research I conducted to try to understand the process by which Alzheimer’s develops. Fortunately, a great deal of research money is currently being spent on Alzheimer’s, but a clearly articulated cause is still elusive. However, many exciting leads are fresh off the press, and the puzzle pieces are beginning to assemble themselves into a coherent story. Researchers are only recently discovering that both fat and cholesterol are severly deficient in the Alzheimer’s brain. It turns out that fat and cholesterol are both vital nutrients in the brain. The brain contains only 2% of the body’s mass, but 25% of the total cholesterol. Cholesterol is essential both in transmitting nerve signals and in fighting off infections.
A crucial piece of the puzzle is a genetic marker that predisposes people to Alzheimer’s, termed “apoE-4.” ApoE plays a central role in the transport of fats and cholesterol. There are currently five known distinct variants of apoE (properly termed “alleles”), with the ones labelled “2”, “3” and “4” being the most prevalent. ApoE-2 has been shown to afford some protection against Alzheimer’s; apoE-3 is the most common “default” allele, and apoE-4, present in 13-15% of the population, is the allele that is associated with increased risk to Alzheimer’s. A person with apoE-4 allele inherited from both their mother and their father has up to a twenty-fold increased likelihood of developing Alzheimer’s disease. However, only about 5% of the people with Alzheimer’s actually have the apoE-4 allele, so clearly there is something else going on for the rest of them. Nonetheless, understanding apoE’s many roles in the body was a key step leading to my proposed low fat/statin theory.
2. Background: Brain Biology 101
Although I have tried to write this essay in a way that is accessible to the non-expert, it will still be helpful to first familiarize you with basic knowledge of the structure of the brain and the roles played by different cell types within the brain.
At the simplest level, the brain can be characterized as consisting of two major components: the gray matter and the white matter. The gray matter comprises the bodies of the neurons, including the cell nucleus, and the white matter contains the myriad of “wires” that connect each neuron to every other neuron it communicates with. The wires are known as “axons” and they can be quite long, connecting, for example, neurons in the frontal cortex (above the eyes) with other neurons deep in the interior of the brain concerned with memory and movement. The axons will figure prominently in the discussions below, because they are coated with a fatty substance called the myelin sheath, and this insulating layer is known to be defective in Alzheimer’s. Neurons pick up signals transmitted through the axons at junctures known as synapses. Here the message needs to be transmitted from one neuron to another one, and various neurotransmitters such as dopamine and GABA exert excitatory or inhibitory influences on signal strength. In adidtion to a single axon, neurons typically have several much shorter nerve fibers called dendrites, whose job is to receive incoming signals from diverse sources. At a given point in time, signals received from multiple sources are integrated in the cell body and a decision is made as to whether the accumulated signal strength is above threshold, in which case the neuron responds by firing a sequence of electrical pulses, which are then transmitted through the axon to a possibly distant destination.
In addition to the neurons, the brain also contains a large number of “helper” cells called glial cells, which are concerned with the care and feeding of neurons. Three principle types of glial cells will play a role in our later discussion: the microglia, the astrocytes, and the oligodendrocytes. Microglia are the equivalent of white blood cells in the rest of the body. They are concerned with fighting off infective agents such as bacteria and viruses, and they also monitor neuron health, making life-and-death decisions: programming a particular neuron for apoptosis (intentional self-destruction) if it appears to be malfunctioning beyond hope of recovery, or is infected with an organism that is too dangerous to let flourish.
The astrocytes figure very prominently in our story below. They nestle up against the neurons and are responsible for assuring an adequate supply of nutrients. Studies on neuron cultures from rodent central nervous systems have shown that neurons depend upon astrocytes for their supply of cholesterol [40]. Neurons critically need cholesterol, both in the synapse [50] and in the myelin sheath [45], in order to successfully transmit their signals, and also as a first line of defense against invasive microbes. Cholesterol is so important to the brain that astrocytes are able to synthesize it from basic ingredients, a skill not found in most cell types. They also supply the neurons with fatty acids, and they are able to take in short chain fatty acids and combine them to form the longer-chain types of fatty acids that are especially prominent in the brain [7][24][36], and then deliver them to neighboring neurons and to the cerebrospinal fluid.
The third type of glial cell is the oligodendrocyte. These cells specialize in making sure the myelin sheath is healthy. Oligodentrocytes synthesize a special sulfur-containing fatty acid, known as sulfatide, from other fatty acids supplied to them by the cerebrospinal fluid [9]. Sulfatide has been shown to be essential for the maintenance of the myelin sheath. Children born with a defect in the ability to metabolize sulfatide suffer from progressive demyelination, and rapid loss of motor and cognitive functions, resulting in an early death before the age of 5 [29]. Depletion in sulfatide is a well-known characterization of Alzheimer’s, even in early stages before it has been manifested as cognitive decline [18]. And ApoE has been shown to play a crucial role in the maintenance of sulfatide [19]. Throughout a person’s life, the myelin sheath has to be constantly maintained and repaired. This is something that researchers are only beginning to appreciate, but two related properties of Alzheimer’s are poor quality myelin sheath alongside a drastically reduced concentration of fatty acids and cholesterol in the cerebrospinal fluid [38].
3. Cholesterol and Lipid Management
In addition to some knowledge about the brain, you will also need to know something about the processes that deliver fats and cholesterol to all the tissues of the body, with a special focus on the brain. Most cell types can use either fats or glucose (a simple sugar derived from carbohydrates) as a fuel source to satisfy their energy needs. However, the brain is the one huge exception to this rule. All cells in the brain, both the neurons and the glial cells, are unable to utilize fats for fuel. This is likely because fats are too precious to the brain. The myelin sheath requires a constant supply of high quality fat to insulate and protect the enclosed axons. Since the brain needs its fats to survive long-term, it is paramount to protect them from oxidation (by exposure to oxygen) and from attack by invasive microbes.
Fats come in all kinds of shapes and sizes. One dimension is the degree of saturation, which concerns how many double bonds they possess, with saturated fats possessing none, monounsaturated fats having only one, and polyunsaturated fats having two or more. Oxygen breaks the double bond and leaves the fat oxidized, which is problematic for the brain. Polyunsaturated fats are thus the most vulnerable to oxygen exposure, because of multiple double bonds.
Fats are digested in the intestine and released into the blood stream in the form of a relatively large ball with a protective protein coat, called a chylomicron. The chylomicron can directly provide fuel to many cell types, but it may also be sent to the liver where the contained fats are sorted out and redistributed into much smaller particles, which also contain substantial amounts of cholesterol. These particles are called “lipoproteins,” (henceforth, LPP’s) because they contain protein in the spherical shell and lipids (fats) in the interior. If you’ve had your cholesterol measured, you’ve probably heard of LDL (low density LPP) and HDL (high density LPP). If you think these are two different kinds of cholesterol, you would be mistaken. They are just two different kinds of containers for cholesterol and fats that serve different roles in the body. There are actually several other LPP’s, for example, VLDL (very-low) and IDL (intermediate), as shown in the accompanying diagram.  In this essay I will refer to these collectively as the XDL’s. As if this weren’t confusing enough, there is also another unique XDL that is found only in the cerebrospinal fluid, that supplies the nutritional needs of the brain and nervous system. This one doesn’t seem to have a name yet, but I will call it “B-HDL,” because it is like HDL in terms of its size, and “B” is for “brain [13]”
In this essay I will refer to these collectively as the XDL’s. As if this weren’t confusing enough, there is also another unique XDL that is found only in the cerebrospinal fluid, that supplies the nutritional needs of the brain and nervous system. This one doesn’t seem to have a name yet, but I will call it “B-HDL,” because it is like HDL in terms of its size, and “B” is for “brain [13]”
An important point about all the XDL’s is that they contain distinctly different compositions, and each is targeted (programmed) for specific tissues. A set of proteins called “apolipoproteins” or, equivalently, “apoproteins” (“apo’s” for short) figure strongly in controlling who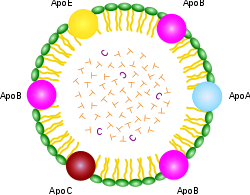 gets what. As you can see from the schematic of the chylomicron shown at the right, it contains a rainbow of different apo’s for every conceivable application. But the XDL’s are far more specific, with HDL containing “A,” LDL containing “B,” VLDL containing “B” and “C,” and IDL containing only “E.” The apo’s have special binding properties that allow the lipid contents to be transported across cell membranes so that the cell can gain access to the fats and choleseterol contained inside.
gets what. As you can see from the schematic of the chylomicron shown at the right, it contains a rainbow of different apo’s for every conceivable application. But the XDL’s are far more specific, with HDL containing “A,” LDL containing “B,” VLDL containing “B” and “C,” and IDL containing only “E.” The apo’s have special binding properties that allow the lipid contents to be transported across cell membranes so that the cell can gain access to the fats and choleseterol contained inside.
The only apo that is of concern to us in the context of this essay is apoE. ApoE is very important to our story because of its known link with Alzheimer’s disease. ApoE is a protein, i.e., sequence of amino acids, and its specific composition is dictated by a corresponding DNA sequence on a protein-coding gene. Certain alterations in the DNA code lead to defects in the ability of the transcribed protein to perform its biological roles. ApoE-4, the allele associated with increased risk to Alzheimer’s, is presumably unable to perform its tasks as efficiently as the other alleles. By understanding what apoE does, we can better infer how the consequences of doing it poorly might impact the brain, and then observe experimentally whether the features of the Alzheimer’s brain are consistent with the roles played by apoE.
A strong clue about apoE’s roles can be deduced from where it is found. As I mentioned above, it is the only apo in both B-HDL in the cerebrospinal fluid and IDL in the blood serum. Only selected cell types can synthesize it, the two most significant of which for our purposes are the liver and the astrocytes in the brain. Thus the astrocytes provide the linkage between the blood and the cerebrospinal fluid. They can usher lipids and cholesterol across the blood-brain barrier, via the special key which is apoE.
It turns out that, although apoE is not found in LDL, it does bind to LDL, and this means that astrocytes can unlock the key to LDL in the same way that they can gain access to IDL, and hence the cholesterol and fatty acid contents of LDL are accessible to astrocytes as well, as long as apoE is functioning properly. The astrocytes reshape and repackage the lipids and release them into the cerebospinal fluid, both as B-HDL and simply as free fatty acids, available for uptake by all parts of the brain and nervous system [13].
One of the critical reshaping steps is to convert the fats into types that are more attractive to the brain. To understand this process you need to know about another dimension of fats besides their degree of saturation, which is their total length. Fats have a chain of linked carbon atoms as their spine, and the total number of carbons in a particular fat characterizes it as short, medium length, or long. The brain works best when the constituent fats are long, and, indeed, the astrocytes are able to take in short chain fats and reorganize them to make longer chain fats [24].
A final dimension of fats that plays a role is where the first double bond is located in a polyunsaturated fat, which distinguishes omega-3 from omega-6 fats (position 3; position 6). Omega-3 fats are very common in the brain. Certain ones of the omega-3 and omega-6 fats are essential fatty acids, in that the human body is unable to synthesize them, and therefore depends upon their supply from the diet. This is why it is claimed that fish “makes you smart”: because cold water fish is the best source of essential omega-3 fats.
Now I want to return to the subject of the XDL’s. It is a dangerous journey from the liver to the brain, as both oxygen and microbes are found in abundance in the blood stream. The XDL’s protective shell contains both LPP’s andunesterified cholesterol, as well as the signature apo that controls which cells can receive the contents, as shown in the accompanying schematic.  The internal contents are esterified cholesterol and fatty acids, along with certain antioxidants that are conveniently being transported to the cells packaged in the same cargo ship. Esterification is a technique to render the fats and cholesterol inert, which helps protect them from oxidation [51]. Having the antioxidants (such as vitamin E and Coenzyme Q10) along for the ride is also convenient, as they too protect against oxidation. The cholesterol contained in the shell, however, is intentionally not esterified, which means that it is active. One of its roles there is to guard against invasive bacteria and viruses [55]. Cholesterol is the first line of defense against these microbes, as it will alert the white blood cells to attack whenever it encounters dangerous pathogens. It has also been proposed that the cholesterol in the XDL’s shell itself acts as an antioxidant [48].
The internal contents are esterified cholesterol and fatty acids, along with certain antioxidants that are conveniently being transported to the cells packaged in the same cargo ship. Esterification is a technique to render the fats and cholesterol inert, which helps protect them from oxidation [51]. Having the antioxidants (such as vitamin E and Coenzyme Q10) along for the ride is also convenient, as they too protect against oxidation. The cholesterol contained in the shell, however, is intentionally not esterified, which means that it is active. One of its roles there is to guard against invasive bacteria and viruses [55]. Cholesterol is the first line of defense against these microbes, as it will alert the white blood cells to attack whenever it encounters dangerous pathogens. It has also been proposed that the cholesterol in the XDL’s shell itself acts as an antioxidant [48].
HDL’s are mostly depleted of the lipid and cholesterol content, and they are tasked with returning the empty shell back to the liver. Once there, cholesterol will be recommissioned to enter the digestive system as part of the bile, which is produced by the gall bladder to help digest ingested fats. But the body is very careful to conserve cholesterol, so that 90% of it will be recycled from the gut back into the blood stream, contained in the chylomicron that began our story about fats.
In summary, the management of the distribution of fats and cholesterol to the cells of the body is a complex process, carefully orchestrated to assure that they will have a safe journey to their destination. Dangers lurk in the blood stream, mostly in the form of oxygen and invasive microbes. The body considers cholesterol to be precious cargo, and it is very careful to conserve it, by recycling it from the gut back to the liver, to be appropriately distributed among the XDL’s that will deliver both cholesterol and fats to the tissues that depend upon them, most especially the brain and nervous system.
4. The Relationship between Cholesterol and Alzheimer’s
Through retrospective studies, the statin industry has been very successful at the game of pretending that benefits derived from high cholesterol are actually due to statins, as I have described at length in an essay on the relationship between statins and fetal damage, sepsis, cancer, and heart failure. In the case of Alzheimer’s, they are playing this game in reverse: they are blaming cholesterol for a very serious problem that I believe is actually caused by statins.
The statin industry has looked long and hard for evidence that high cholesterol might be a risk factor for Alzheimer’s. They examined cholesterol levels for men and women of all ages between 50 and 100, looking back 30 or more years if necesssary, to see if there was ever a correlation between high cholesterol and Alzheimer’s. They found only one statistically significant relationship: men who had had high cholesterol in their 50’s had an increased susceptibility to Alzheimer’s much later in life [3].
The statin industry has jumped on this opportunity to imply that high cholesterol might cause Alzheimer’s, and, indeed, they have been very fortunate in that reporters have taken the bait and are promoting the idea that, if high cholesterol many years ago is linked to Alzheimer’s, then statins might protect from Alzheimer’s. Fortunately, there exist lengthy web pages (Cholesterol Doesn’t Cause Alzheimer’s) that have documented the long list of reasons why this idea is absurd.
Men who have high cholesterol in their 50’s are the poster child for statin treatment: all of the studies that have shown a benefit for statins in terms of reducing the number of minor heart attacks involved men in their 50’s. High cholesterol is positively correlated with longevity in people over 85 years old [54], and has been shown to be associated with better memory function [53] and reduced dementia [35]. The converse is also true: a correlation between falling cholesterol levels and Alzheimer’s [39]. As will be discussed further later, people with Alzheimer’s also have reduced levels of B-HDL, as well as sharply reduced levels of fatty acids, in the cerbrospinal fluid, i.e, impoverished supply of cholesterol and fats to the myelin sheath [38]. As we saw earlier, fatty acid supply is essential as building blocks for the sulfatide that is synthesized by oligodendrocytes to keep the myelin sheath healthy [29].
The obvious study that needs to be done is to bin the men who had high cholesterol in their 50’s into three groups: those who never took statins, those who took smaller doses for shorter times, and those who took larger doses for longer times. Such a study would not be hard to do; in fact, I suspect something like it has already been done. But you’ll never hear about it because the statin industry has buried the results.
In a very long term retrospective cohort study of members of the Permanente Medical Care Program in northern California, researchers looked at cholesterol data that were obtained between 1964 and 1973 [46]. They studied nearly ten thousand people who had remained members of that health plan in 1994, upon the release of computerized outpatient diagnoses of dementia (both Alzheimer’s and vascular dementia). The subjects were between 40 and 45 years old when the cholesterol data were collected.
The researchers found a barely statistically significant result that people who were diagnosed with Alzheimer’s had higher cholesterol in their 50’s than the control group. The mean value for the Alzheimer’s patients was 228.5, as against 224.1 for the controls.
The question that everybody ought to be asking is: for the Alzheimer’s group, how did the people who later took statins stack up against the people who didn’t? In extreme understatement, the authors offhandedly remark in the middle of a paragraph: “Information on lipid-lowering treatments, which have been suggested to decrease dementia risk [31], was not available for this study.” You can be sure that, if there was any inkling that the statins might have helped, these researchers would have been allowed access to those data.
The article they refer to for support, reference [19] in [46] (which is reference [44] here) was very weak. The abstract for that article is repeated in full here in the Appendix. But the concluding sentence sums it up well: “A more than a modest role for statins in preventing AD [Alzheimer’s Disease] seems unlikely.” This is the best they can come up with to defend the position that statins might protect from Alzheimer’s.
An intuitive explanation for why high cholesterol at an early age might be correlated with Alzheimer’s risk has to do with apoE-4. People with that allele are known to have high cholesterol early in life [39], and I believe this is a protective strategy on the part of the body. The apoE-4 allele is likely defective in the task of importing cholesterol into the astrocytes, and therefore an increase in the bioavailability of cholesterol in blood serum would help to offset this deficit. Taking a statin would be the last thing a person in that situation would want to do.
5. Do Statins Cause Alzheimer’s?
There is a clear reason why statins would promote Alzheimer’s. They cripple the liver’s ability to synthesize cholesterol, and as a consequence the level of LDL in the blood plummets. Cholesterol plays a crucial role in the brain, both in terms of enabling signal transport across the synapse [50] and in terms of encouraging the growth of neurons through healthy development of the myelin sheath [45]. Nonetheless, the statin industry proudly boasts that statins are effective at interfering with cholesterol production in the brain [31][47] as well as in the liver.
Yeon-Kyun Shin is an expert on the physical mechanism of cholesterol in the synapse to promote transmission of neural messages, and one of the authors of [50] referenced earlier. In an interview by a Science Daily reporter, Shin said: “If you deprive cholesterol from the brain, then you directly affect the machinery that triggers the release of neurotransmitters. Neurotransmitters affect the data-processing and memory functions. In other words — how smart you are and how well you remember things.”
A recent review of two large population-based double-blind placebo-controlled studies of statin medications in individuals at risk for dementia and Alzheimer disease showed that statins are not protective against Alzheimer’s [34]. The lead author of the study, Bernadette McGuinness, was quoted by a reporter from Science Daily as saying, “From these trials, which contained very large numbers and were the gold standard — it appears that statins given in late life to individuals at risk of vascular disease do not prevent against dementia.” A researcher at UCLA, Beatrice Golomb, when asked to comment on the results, was even more negative, saying, “Regarding statins as preventive medicines, there are a number of individual cases in case reports and case series where cognition is clearly and reproducibly adversely affected by statins.” In the interview, Golomb remarked that various randomized trials have shown that statins were either adverse or neutral towards cognition, but none have shown a favorable response.
A common side effect of statins is memory dysfunction. Dr. Duane Graveline, fondly known as “spacedoc” because he served as a doctor to the astronauts, has been a strong advocate against statins and is collecting evidence of statin side effects directly from statin users around the world. He was led to this assault on statins as a consequence of his own personal experience of transient global amnesia, a frightening episode of total memory loss which he is convinced was caused by the statin drugs he was taking at the time. He has now completed three books describing a diverse collection of damning side effects of statins, the most famous of which is Lipitor: Thief of Memory [17].
A second way (besides their direct impact on cholesterol) in which statins likely impact Alzheimer’s is in their indirect negative effect on the supply of fatty acids and antioxidants to the brain. It is a given that statins drastically reduce the level of LDL in the blood serum. This is their claim to fame. It is interesting, however, that they succeed in reducing not just the amount of cholesterol contained in the LDL particles, but rather the actual number of LDL particles altogether. This means that, in addition to depleting cholesterol, they reduce the available supply to the brain of both fatty acids and antixodiants, which are also carried in the LDL particles. As we’ve seen, all three of these substances are essential to proper brain functioning.
I conjecture that the reasons for this indirect effect are two-fold: (1) there is inadequate cholesterol in the bile to metabolize dietary fats, and (2) the rate-limiting effect on the production of LDL is the ability to provide adequate cholesterol in the shell to assure survival of the contents during transport in the blood stream; i.e., to protect the contents from oxidation and marauding bacteria and viruses. People who take the highest 80 mg/dl dosage of statins often end up with LDL levels as low as 40mg/dl, well below even the lowest numbers observed naturally. I shudder to think of the probable long-term consequences of such severe depletion in fats, cholesterol, and antioxidants.
A third way in which statins may promote Alzheimer’s is by crippling the ability for cells to synthesize coenzyme Q10. Coenzyme Q10 has the misfortune of sharing the same metabolic pathway as cholesterol. Statins interfere with a crucial intermediate step on the pathway to the synthesis of both cholesterol and coenzyme Q10. Coenzyme Q10 is also known as “ubiquinone” because it seems to show up everywhere in cell metabolism. It is found both in the mitochondria and in the lysosomes, and its critical role in both places is as an antioxidant. The inert esters of both cholesterol and fatty acids are hydrolyzed and activated in the lysosomes [8], and then released into the cytoplasm. Coenzyme Q10 consumes excess oxygen to keep it from doing oxidative damage [30], while also generating energy in the form of ATP (adenosine triphosphate, the universal energy currency in biology).
The final way in which statins should increase Alzheimer’s risk is through their indirect effect on vitamin D. 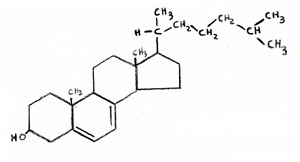 Vitamin D is synthesized from cholesterol in the skin, upon exposure to UV rays from the sun. In fact, the chemical formula of vitamin D is almost indistinguishable from that of cholesterol, as shown in the two attached figures (cholesterol on the left, vitamin D on the right). If LDL levels are
Vitamin D is synthesized from cholesterol in the skin, upon exposure to UV rays from the sun. In fact, the chemical formula of vitamin D is almost indistinguishable from that of cholesterol, as shown in the two attached figures (cholesterol on the left, vitamin D on the right). If LDL levels are  kept artificially low, then the body will be unable to resupply adequate amounts of cholesterol to replenish the stores in the skin once they have been depleted. This would lead to vitamin D deficiency, which is a widespread problem in America.
kept artificially low, then the body will be unable to resupply adequate amounts of cholesterol to replenish the stores in the skin once they have been depleted. This would lead to vitamin D deficiency, which is a widespread problem in America.
It is well known that vitamin D fights infection. To quote from [25], “Patients with severe infections as in sepsis have a high prevalence of vitamin D deficiency and high mortality rates.” As will be elaborated on later, a large number of infective agents have been shown to be present in abnormally high amounts in the brains of Alzheimers patients [27][26].
Dr. Grant has recently argued [16] that there are many lines of evidence pointing to the idea that dementia is associated with vitamin D deficiency. An indirect argument is that vitamin D deficiency is associated with many conditions that in turn carry increased risk for dementia, such as diabetes, depression, osteoporosis, and cardiovascular disease. Vitamin D receptors are widespread in the brain, and it is likely that they play a role there in fighting off infection. Vitamin D surely plays other vital roles in the brain as well, as powerfully suggested by this quote taken from the abstract of [32]: “We conclude there is ample biological evidence to suggest an important role for vitamin D in brain development and function.”
6. Astrocytes, Glucose Metabolism, and Oxygen
Alzheimer’s is clearly correlated with a deficiency in the supply of fat and cholesterol to the brain. IDL, when functioning properly, is actually incredibly efficient in cholesterol and fat throughput from the blood across cell membranes, compared to LDL [8]. It gives up its contents much more readily than the other apo’s. And it achieves this as a direct consequence of apoE. IDL (as well as LDL) in the blood delivers fats and cholesterol to the astrocytes in the brain, and the astrocytes can thus use this external source instead of having to produce these nutrients themselves. I suspect, in fact, that astrocytes only produce a private supply when the external supply is insufficient, and they do so reluctantly.
Why would it be disadvantageous for an astrocyte to synthesize its own fats and cholesterol? In my opinion, the answer has to do with oxygen. An astrocyte needs a significant energy source to synthesize fats and cholesterol, and this energy is usually supplied by glucose from the blood stream. Furthermore, the end-product of glucose metabolism is acetyl-Coenzyme A, the precursor to both fatty acids and cholesterol. Glucose can be consumed very efficiently in the mitochondria, internal structures within the cell cytoplasm, via aerobic processes that require oxygen. The glucose is broken down to produce acetyl-Coenzyme A as an end-product, as well as ATP, the source of energy in all cells.
However, oxygen is toxic to lipids (fats), because it oxidizes them and makes them rancid. Lipids are fragile if not encased in a protective shell like IDL, HDL, or LDL. Once they are rancid they are susceptible to infection by invasive agents like bacteria and viruses. So an astrocyte trying to synthesize a lipid has to be very careful to keep oxygen out, yet oxygen is needed for efficient metabolism of glucose, which will provide both the fuel (ATP) and the raw materials (acetyl-Coenzyme A) for fat and cholesterol synthesis.
What to do? Well, it turns out that there is an alternative, although much less efficient, solution: to metabolize glucose anaerobically directly in the cytoplasm. This process does not depend on oxygen (a great advantage) but it also yields substantially less ATP (only 6 ATP as contrasted with 30 if glucose is metabolized aerobically in the mitochondria). The end product of this anaerobic step is a substance called pyruvate, which could be further broken down to yield a lot more energy, but this process is not accessible to all cells, and it turns out that the astrocytes need help for this to happen, which is where amyloid-beta comes in.
7. The Crucial Role of Amyloid-Beta
Amyloid-beta (also known as “abeta”) is the substance that forms the famous plaque that accumulates in the brains of Alzheimer’s patients. It has been believed by many (but not all) in the research community that amyloid-beta is the principal cause of Alzheimer’s, and as a consequence, researchers are actively seeking drugs that might destroy it. However, amyloid-beta has the unique capability of stimulating the production of an enzyme, lactate dehydrogenase, which promotes the breakdown of pyruvate (the product of anaerobic glucose metabolism) into lactate, through an anaerobic fermentation process, with the further production of a substantial amount of ATP.
The lactate, in turn, can be utilized itself as an energy source by some cells, and it has been established that neurons are on the short list of cell types that can metabolize lactate. So I conjecture that the lactate is transported from the astrocyte to a neighboring neuron to enhance its energy supply, thus reducing its dependence on glucose. It is also known that apoE can signal the production of amyloid-beta, but only under certain poorly understood environmental conditions. I suggest those environmental triggers have to do with the internal manufacture of fats and cholesterol as opposed to the extraction of these nutrients from the blood supply. I.e., amyloid-beta is produced as a consequence of environmental oxidative stress due to an inadequate supply of fats and cholesterol from the blood.
In addition to being utilized as an energy source by being broken down to lactate, pyruvate can also be used as a basic building block for synthesizing fatty acids. So anaerobic glucose metabolism, which yields pyruvate, is a win-win-win situation: (1) it significantly reduces the risk of exposure of fatty acids to oxygen, (2) it provides a source of fuel for neighboring neurons in the form of lactate, and (3) it provides a basic building block for fatty acid synthesis. But it depends upon amyloid-beta to work.
Thus, in my view (and in the view of others [28] [20] Amyloid-Beta and Alzheimer’s), amyloid-beta is not a cause of Alzheimer’s, but rather a protective device against it. The abstract of reference [28] arguing this point of view is reproduced in full in the Appendix. Several variants of a genetic defect associated with amyloid precursor protein (APP), the protein from which amyloid-beta is derived, have now been identified. A defect in this protein, which is associated with an increased risk of early onset Alzheimer’s, would likely lead to a reduced ability to synthesize amyloid-beta, which would then leave the brain with a big problem, since both the fuel and the basic building blocks for fatty acid synthesis would be in short supply, while oxygen trekking through the cell to the mitochondria would be exposing whatever fats were being synthesized to oxidation. The cell would likely be unable to keep up with need, and this would lead to a reduction in the number of fatty acids in the Alzheimer’s cerebrospinal fluid, a well-established characteristic of Alzheimer’s [38].
8. Cholesterol’s Role in the Brain
The brain comprises only 2% of the body’s total weight, yet it contains nearly 25% of the total cholesterol in the body. It has been determined that the limiting factor allowing the growth of synapses is the availability of cholesterol, supplied by the astrocytes. Cholesterol plays an incredibly important role in the synapse, by shaping the two cell membranes into a snug fit so that the signal can easily jump across the synapse [50]. So inadequate cholesterol in the synapse will weaken the signal at the outset, and inadequate fat coating the myelin sheath will further weaken it and slow it down during transport. A neuron that can’t send its messages is a useless neuron, and it only makes sense to prune it away and scavenge its contents.
The neurons that are damaged in Alzheimer’s are located in specific regions of the brain associated with memory and high level planning. These neurons need to transmit signals long distances between the frontal and prefrontal cortex and the hippocampus, housed in the midbrain. The transport of these signals depends on a strong and tight connection in the synapse, where the signal is transferred from one neuron to another, and a secure transmission across the long nerve fiber, a part of the white matter. The myelin sheath which coats the nerve fiber consists mainly of fatty acids, along with a substantial concentration of cholesterol. If it is not well insulated, the signal transmission rate will slow down and the signal strength will be severely reduced. Cholesterol is crucial for the myelin as well as for the synapse, as demonstrated dramatically through experiments conducted on genetically defective mice by Gesine Saher et al. [45]. These mutant mice lacked the ability to synthesize cholesterol in myelin-forming oligodendrocytes. They had severly disturbed myelin in their brains, and exhibited ataxia (uncoordinated muscle movements) and tremor. In the abstract, the authors wrote unequivocally, “This shows that cholesterol is an indispensable component of myelin membranes.”
In a post-mortem study comparing Alzheimer’s patients with a control group without Alzheimer’s, it was found that the Alzheimer’s patients had significantly reduced amounts of cholesterol, phospholipids (e.g, B-HDL), and free fatty acids in the cerebrospinal fluid than did the controls [38]. This was true irrespective of whether the Alzheimer’s patients were typed as apoE-4. In other words, reductions in these critical nutrients in the spinal fluid are associated with Alzheimer’s regardless of whether the reduction is due to defective apoE. The reductions in fatty acids were alarming: 4.5 micromol/L in the Alzheimer’s patients, compared with 28.0 micromol/L in the control group. This is a reduction by more than a factor of 6 in the amount of fatty acid available to repair the myelin sheath!
People with the apoE-4 allele tend to have high serum cholesterol. The question of whether this high cholesterol level might be an attempt on the part of the body to adjust for a poor rate of cholesterol uptake in the brain was addressed by a team of researchers in 1998 [39]. They studied 444 men between 70 and 89 years old at the time, for whom there existed extensive records of cholesterol levels dating back to several decades ago. Most significantly, cholesterol levels fell for the men who developed Alzheimer’s prior to their showing Alzheimer’s symptoms. The authors suggested that their high cholesterol might have been a protective mechanism against Alzheimer’s.
One might wonder why their cholesterol levels fell. There was no mention of statin drugs in the article, but statins would certainly be an effective way to reduce cholesterol levels. The statin industry would like people to believe that high cholesterol is a risk factor for Alzheimer’s, and they are quite thrilled that high cholesterol early in life is correlated with Alzheimer’s much later. But these results suggest quite the opposite: that blood cholesterol levels are kept high intentionally by the body regulatory mechanisms in an attempt to compensate for the defect. A high concentration will lead to an increase in the rate of delivery to the brain, where it is critically needed to keep the myelin sheath healthy and to promote neuron signaling in the synapses.
Using MRI technology, researchers at UCLA were able to measure the degree of breakdown of myelin in specific regions of the brain [6]. They conducted their studies on over 100 people between 55 and 75 years old, for whom they also determined the associated apoE allele (2, 3, or 4). They found a consistent trend in that apoE-2 had the least amount of degradation, and apoE-4 had the most, in the frontal lobe region of the brain. All of the people in the study were thus far healthy with respect to Alzheimer’s. These results show that premature breakdown of myelin sheath (likely due to an insufficient supply of fats and cholesterol to repair it) is associated with apoE-4.
To summarize, I hypothesize that, for the apoE-4 Alzheimer’s patients, defective apoE has led to an impaired ability to transport fats and cholesterol from the blood stream, via the astrocytes, into the cerebrospinal fluid. The associated high blood serum cholesterol is an attempt to partially correct for this defect. For the rest of the Alzheimer’s patients (the ones without the apoE-4 allele but who also have severely depleted fatty acids in their cerebrospinal fluid), we have to look for another reason why their fatty acid supply chain might be broken.
9. Infections and Inflammation
To summarize what I have said so far, Alzheimer’s appears to be a consequence of an inability of neurons to function properly, due to a deficiency in fats and cholesterol. A compounding problem is that the fats over time will become rancid if they cannot be adequately replenished. Rancid fats are vulnerable to attack by microorganisms such as bacteria and viruses. Amyloid-beta is part of the solution because it allows the astrocytes to be much more effective in utilizing glucose anaerobically, which protects the internally synthesized fats and cholesterol from toxic oxygen exposure, while at the same time providing the energy needed both by the astrocyte for the synthesis process and by neighboring neurons to fuel their signal firings.
Besides the astrocytes, the microglia in the brain are also implicated in Alzheimer’s. Microglia promote neuron growth when all is well, but trigger neuron programmed cell death in the presence of toxic substances secreted by bacteria such as polysaccharides [56]. Microglia will defensively secrete cytokines (communication signals that promote an immune response) when exposed to infective agents, and these in turn will lead to inflammation, another well-known feature associated with Alzheimer’s [1]. The microglia are able to control whether neurons should live or die, and they surely base this decision on factors related to how well the neuron functions and whether it is infected. Once enough neurons have been programmed for cell death, the disease will manifest itself as cognitive decline.
10. Evidence that Infection is Associated with Alzheimer’s
There is substantial evidence that Alzheimer’s is related to an increased likelihood of infective agents appearing in the brain. Some researchers believe that infective agents are the principle cause of Alzheimer’s. There are a number of bacteria that reside in the human digestive system and can co-exist with our own cells without any harm. However, H. pylori, one that is quite common, has been recently shown to be responsible for stomach ulcers. It has been suspected that H. Pylori might be implicated in Alzheimer’s, and, indeed, a recent study showed that Alzheimer’s patients had a significantly higher concentration of an antibody against H. Pylori in both their cerebrospinal fluid and their blood than non-Alzheimer’s controls [26]. H. pylori was detected in 88% of the Alzheimer’s patients but only 47% of the controls. In an effort to treat the Alzheimer’s patients, the researchers administered a potent combination of antibiotics, and assessed the degree of mental decline over the next two years [27]. For 85% of the patients, the infection was successfully routed, and for those patients, cognitive improvement was also detected after two years had elapsed. So this was a nice example of the possibility of treating Alzheimer’s through antibiotics.
C. pneumoniae is a very common bacterium, estimated to infect 40-70% of adults. But there’s a big difference between a bacterium being in the blood stream and making its way into the inner sanctum of the brain. A study of post-mortem samples from various regions of the brains of Alzheimer’s patients and non-Alzheimer’s controls revealed a remarkably different statistic: 17 out of 19 Alzheimer’s brains tested positive for the bacterium, whereas only 1 out of 19 brains from the control group tested positive [5].
Many other infective agents, both viruses and bacteria, have been found to be associated with Alzheimer’s, including herpes simplex virus, picornavirus, Borna disease virus, and spirochete [23]. One proposal was that a particularbacteriophage — a virus that infects the bacterium C. pneumoniae — might be responsible for Alzheimer’s [14]. The authors argued that the phages might make their way into the mitochondria of the host cell and subsequently initiate Alzheimer’s.
11. Ketogenic Diet as Treatment for Alzheimer’s
One of the promising new treatment paradigms for Alzheimer’s is to have the patient switch to an extremely high fat, low carb diet, a so-called “ketogenic” diet. The name comes from the fact that the metabolism of dietary fats produces “ketone bodies” as a by-product, which are a very useful resource for metabolism in the brain. It is becoming increasingly clear that defective glucose metabolism in the brain (so-called “type-3 diabetes”) is an early characteristic of Alzheimer’s. Ketone bodies, whether they enter the astrocyte directly or are produced in the astrocyte itself by breaking down fats, can be delivered to adjacent neurons, as shown in the accompanying figure.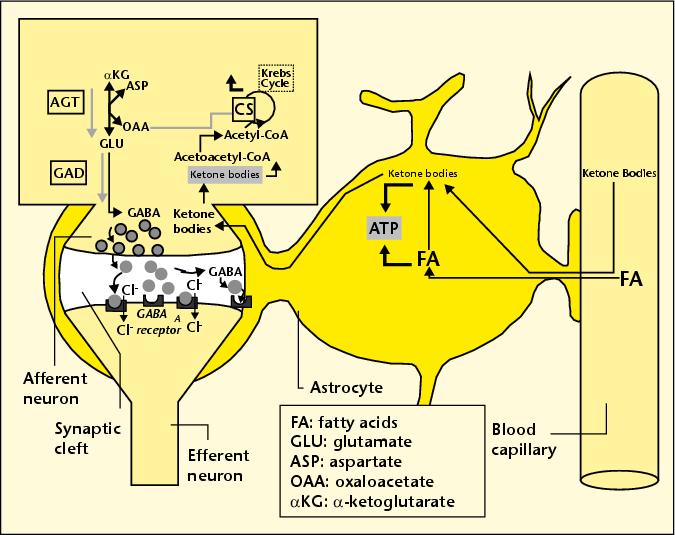 These neurons can utilize the ketone bodies both as an energy source (replacing and therefore relieving glucose) and as a precursor to GABA, a critical neurotransmitter that is widespread in the brain.
These neurons can utilize the ketone bodies both as an energy source (replacing and therefore relieving glucose) and as a precursor to GABA, a critical neurotransmitter that is widespread in the brain.
Evidence that a ketogenic diet might help Alzheimer’s was first found through research conducted on mice who had been bred to be prone to Alzheimer’s disease [21]. Researchers found that the mice’s cognition improved when they were treated with a high-fat low-carb diet, and also that the amount of amyloid-beta in their brain was reduced. The latter effect would be anticipated based on the premise that amyloid-beta promotes full utilization of glucose anaerobically, as I discussed previously. By having ketone bodies as an additional source of fuel, the dependence on glucose is reduced. But another effect that may be more important than this is the availability of high-quality fats to improve the condition of the myelin sheath.
This idea is supported by other experiments done on human Alzheimer’s patients [11] [42]. A placebo-controlled 2004 study [42] of the effect of dietary fat enrichment on Alzheimer’s is especially informative, because it uncovered a significant difference in effectiveness for the fat-enrichment for subjects who did not have the apoE-4 allele as compared with those who did. The experimental test group were given a supplemental drink containing emulsified medium chain triglycerides, found in high concentration in coconut oil. The subjects without the apoE-4 allele showed a significant improvement in score on a standard test for Alzheimer’s, whereas those with the apoE-4 allele did not. This is a strong indicator that the benefit may have to do with an increase in uptake by the astrocyte of these high-quality fats, something that the subjects with the apoE-4 allele are unable to accomplish due to the defective IDL and LDL transport mechanisms.
12. NADH Treatment: the Crucial Role of Antioxidants
One of the very few promising treatments for Alzheimer’s is the coenzyme, NADH (nicotinamide adenine dinucleotide) [12]. In a placebo-controlled study, Alzheimer’s subjects given NADH for six months exhibited significantly better performances on verbal fluency, visual constructional ability and abstract verbal reasoning than the control subjects given a placebo.
Why would NADH be effective? In the process of converting pyruvate to lactate, lactate dehydrogenase consumes oxygen by oxidizing NADH to NAD+, as illustrated in the accompanying figure. So, if the bioavailability of NADH is increased, it stands to reason that the astrocyte would have an enhanced ability to convert pyruvate to lactate, the critical step in the anaerobic metabolic pathway that is enhanced by amyloid-beta. The process, by absorbing the toxic oxygen, would reduce the damage to the lipids due to oxygen exposure, and would also provide lactate as a source of energy for the neurons.
13. Excessive Oxygen Exposure and Cognitive Decline
It has been observed that some elderly people suffer temporary and sometimes permanent cognitive decline following a lengthy operation. Researchers at the University of South Florida and Vanderbilt University suspected that this might be due to excessive exposure to oxygen [4]. Typically, during an operation, people are often administered high doses of oxygen, even as much as 100% oxygen. The researchers conducted an experiment on young adult mice, which had been engineered to be predisposed towards Alzheimer’s but had not yet suffered cognitive decline. They did however already have amyloid-beta deposits in their brains. The re-engineered mice, as well as a control group that did not have the Alzheimer’s susceptibility gene, were exposed to 100-percent oxygen for a period of three hours, three times over the course of several months, simulating repeated operations. They found that the Alzheimer’s pre-disposed mice suffered significant cognitive decline following the oxygen exposure, by contrast with the control mice.
This is a strong indication that the excessive oxygen exposure during operations is causing oxidative damage in the Alzheimer’s brain. Given the arguments I have presented above, this result makes good sense. The brain, by converting to anaerobic metabolism for generating energy (with help from amyloid-beta) is trying its best to avoid exposing the fatty acids and cholesterol to oxidative damage. But an extremely high concentration of oxygen in the blood makes it very difficult to protect the fats and cholesterol during transport through the blood, and also probably causes an unavoidable increase in oxygen uptake and therefore exposure within the brain itself.
14. Fats are a Healthy Choice!
You would practically have to be as isolated as an Australian Aborigine not to have absorbed the message that dietary fats, particularly saturated fats, are unhealthy. I am extremely confident that this message is false, but it is nearly impossible to turn the opinion tide due to its pervasive presence. Most people don’t question why fats are bad; they assume that researchers must have done their homework, and they trust the result.
To say that the current situation with regard to dietary fats is confusing would be an understatement. We are repeatedly told to keep our total fat intake down to, ideally, 20% of our total calories. This is difficult to achieve, and I believe it is misguided advice. In direct contradiction to this “low-fat” goal, we are encouraged to consume as much as possible of the “good” kinds of fats. Fortunately, the message is finally becoming widely embraced that omega-3 fats are healthy and that trans fats are extremely unhealthy. DHA (docosahexaenoic acid) is an omega-3 fat that is found in large quantities in the healthy brain. In the diet, it is available mainly from cold water fish, but eggs and dairy are also good sources. Trans fats are generated by a high-heat process that hydrolyzes polyunsaturated fats into a more stable configuration, which increases their shelf life but makes them so unnatural they almost can no longer be called a food. Trans fats are extremely damaging both to heart and brain health. A high consumption of trans fats has recently been shown to increase the risk of Alzheimer’s [41]. Trans fats are especially prevalent in highly processed foods — particularly when fats are converted to a powdered form.
We are told to avoid saturated fats, mainly because they have appeared, from empirical evidence, to be more likely to raise LDL levels than unsaturated fats. Yet these fats are less susceptible to oxidation, and this may be why they show up in LDL — because they are of higher quality and therefore should preferentially be delivered to the tissues for functional roles rather than as fuel (i.e., free fatty acids). Coconut oil, a saturated fat, has been shown to benefit Alzheimer’s patients [42]. And high-fat dairy (also highly saturated) has been shown to be beneficial both to fertility among women [10] and, remarkably, to heart disease [37][22].
Despite the widespread belief that fats (particularly saturated fats) are unhealthy, an article that appeared in the American Journal of Clinical Nutrition in 2004 [37] claims that, for a group of post-menopausal women, a high-fat, high-saturated-fat diet affords better protection from coronary artery disease than a low-fat (25% of calories from fats) diet. The subjects in the study were obese women with coronary artery disease. Most of them had high blood pressure, and many had diabetes. They fit the profile for metabolic syndrome that I have previously argued is a direct consequence of a prolonged low-fat high-carb diet. I am gratified to see that my hypothesis that an increase in fat intake would decrease their risk of heart disease has been verified by a carefully controlled study.
Another investigation where fats were shown to afford protection against heart disease has just been completed. It involved a long-term study of a large number of Swedish men [22]. The authors looked at low- vs high-fat dairy, as well as consumption of fruits and vegetables, meats, grains, etc. The only statistically significant result that afforded protection from heart disease was a combination of high-fat dairy and lots of fruits and vegetables. Fruits and vegetables with low-fat dairy afforded no protection.
I suspect one of the critical nutrients the fruits and vegetables provide is antioxidants that help prolong the life of the fats. Other excellent sources of antioxidants include richly colored fruits like berries and tomatoes, coffee, green tea, and dark chocolate, and several spices, most especially cinnamon and turmeric (a major ingredient of curry). These should be consumed in abundance along with fats for optimal results.
Polyunsaturated fats such as corn oil and canola oil are unhealthy for the brain precisely because they are unsaturated. There are two major problems: (1) they have a low melting point, which means that, if they are used for frying they will be converted to trans fats, which are extremely unhealthy, and (2) they are much more susceptible to becoming rancid (oxidized) at room temperature than saturated fats, i.e., they have a shorter shelf life.
Researchers in Germany recently conducted an ingenious experiment designed to determine how the degree of freshness of polyunsaturated fats affects the metabolism of those fats in female lactating rats [43]. They divided female rats into two groups, and the only difference between the test group and the controls was that the test group was given fats that had been left in a relatively warm place for 25 days, which caused considerable oxidative damage, whereas the controls were fed fresh fats instead. The rats’ unusual diet was begun on the day that they gave birth to a litter. The researchers examined the mammary glands and the milk produced by the two groups for apparent differences. They found that the test group’s milk was markedly reduced in the amount of fat it contained, and their mammary glands correspondingly took up less fat from the blood supply. One might surmise that the rats’ metabolic mechanisms were able to detect oxidative damage to the fats, and therefore rejected them, prefering to do without rather than to risk the consequences of feeding their pups oxidized fats. Consequently, the pups of the test group gained significantly less weight than the control group’s pups.
Boxed items like cookies and crackers that contain processed polyunsaturated fats are doctored with antioxidants and even antibiotics to protect them from spoiling. Once they’re consumed, however, they still have to be protected from going rancid. Biochemical laws work the same way whether inside or outside the body. There are plenty of bacteria throughout the body that would be eager to take up house-keeping in rancid fats. The body has devised all kinds of strategies for protecting fats from oxidation (becoming rancid) and from attack by bacteria. But its task is rendered much easier for saturated rather than unsaturated fats, and for fresh rather than stale fats.
If we stop trying to get by on as few fats as possible in the diet, then we don’t have to become so preoccupied with getting the “right” kinds of fats. If the body is supplied with an overabundance of fats, it can pick and choose to find the perfect fat to match each particular need; excess or defective fats can just be used as fuel, where it’s not very important which fat it is, as long as it can be broken down to release energy.
15. Summary and Conclusion
This is an exciting time for Alzheimer’s research, as new and surprising discoveries are coming out at a rapid pace, and evidence is mounting to support the notion that Alzheimer’s is a nutritional deficiency disease. It is an indication of how much progress has been made in recent years to note that 42% of the references in this essay were published in 2008 or 2009. A popular new theory is that Alzheimer’s may grow out of an impaired ability to metabolize glucose in the brain. The term “type-3 diabetes” has been coined to describe this defect, which often appears long before any symptoms of Alzheimer’s [49]. A shift from aerobic towards anaerobic glucose metabolism in the brain seems to be a harbinger of Alzheimer’s later in life, but I argue that the reason for this shift is both to provide a basic ingredient (pyruvate) from which to synthesize fatty acids, while simultaneously protecting them from potentially damaging oxidation. The ApoE-4 allele, which is associated with increased risk to Alzheimer’s, clearly implicates defects in fat and cholesterol transport, and the remarkable 6-fold reduction in the amount of fatty acids present in the cerebrospinal fluid of Alzheimer’s patients [38] speaks loudly the message that fat insufficiency is a key part of the picture. The observation that the myelin is degraded in the frontal lobes of the brains of people possessing the apoE-4 allele further substantiates the theory that the myelin repair mechanism is defective.
Cholesterol obviously plays a vital role in brain function. A whopping 25% of the total cholesterol in the body is found in the brain, and it is present in abundance both in the synapses and in the myelin sheath. The cholesterol in both of these places has been shown to play an absolutely essential role in signal transport and in growth and repair.
Given the strong positive role played by cholesterol, it can only be assumed that statin drugs would increase the risk of developing Alzheimer’s. However, the statin industry has been remarkably successful thus far in hiding this painful fact. They have managed to make much of the observation that high cholesterol much earlier in life is associated with an increased risk to Alzheimer’s thirty years later. Yet they offer not a single study, not even a retrospective study, to substantiate any claim that actively reducing cholesterol through statin therapy would improve the situation for these people. In fact, most damningly, the statin usage evidence that would answer the question was “unavailable” to the researchers who conducted the seminal study.
Beatrice Golomb is an M.D. Ph.D. who heads up the UCSD Statin Study group, a research team who are actively investigating the risk-benefit balance of statin drugs. She is increasingly becoming convinced that statin drugs should not be recommended for the elderly: that in their case the risks clearly outweigh the benefits. She makes a strong case for this position in an on-line article available here [15]. The section on Alzheimer’s is particularly compelling, and it points out the pitfalls in relying on previous studies done by the statin industry, where often those who have memory problems as side-effects of the statin drugs are excluded from the study, so that the results end up inappropriately biased in favor of statins. In summary, she wrote: “It must be emphasized that the randomized trial evidence has, to date, uniformly failed to show cognitive benefits by statins and has supported no effect or frank and significant harm to cognitive function.”
In addition to refusing to take statin therapy, another way in which an individual can improve their odds against Alzheimer’s is to consume plenty of dietary fats. It seems odd to suddenly switch from a “healthy” low-fat diet to an extremely high fat ketogenic diet, once a diagnosis of Alzheimer’s is made. A ketogenic diet consists, ideally, of 88% fat, 10% protein, and 2% carbohydrate [11]. That is to say, it is absurdly high in fat content. It seems much more reasonable to aim for something like 50% fat, 30% protein, and 20% carbohydrate, so as to pro-actively defend against Alzheimer’s.
I highly recommend a recent book written by the pediatric brain surgeon, Larry McCleary, M.D., called The Brain Trust Program [33]. This book gives a wealth of fascinating information about the brain, as well as specific recommendations for ways to improve cognitive function and avert later Alzheimer’s. Most significantly, he recommends a diet that is high in cholesterol and animal fats, including an abundance of fish, seafood, meat, and eggs. He also recommends coconuts, almonds, avocados and cheese, all foods that contain a significant amount of fat, while encouraging the avoidance of “empty carbs.” His knowledge on this subject grew out of his interest in helping his young patients heal more rapidly after brain trauma.
Our nation is currently bracing itself for an onslaught of Alzheimer’s, at a time when baby boomers are approaching retirement, and our health care system is already in a crisis of escalating costs and shrinking funds. We can not afford the high cost of caring for the swelling population of Alzheimer’s patients that our current practices of low-fat diet and ever expanding statin usage are promoting.
Appendix In this appendix, I include the full abstract of two papers that are relevant to the theory presented here. The first is the abstract of reference [19] in [46], which is reference [44] here [see the section on statin drugs above for context]:
Abstract, “Epidemiological and clinical trials evidence about a preventive role for statins in Alzheimer’s disease:”
“This paper reviews epidemiological and clinical trials data about whether statin use reduces the risk of Alzheimer’s disease (AD). The available information has come in three waves. The initial, mostly cross-sectional observational reports suggested that statins might prevent dementia. Next, two large clinical trials with cognitive add-on studies showed no benefit and neither did the third wave, again with observational studies. The latter were mostly longitudinal, and were critical of the first studies for not adequately addressing confounding by indication (i.e. that patients with dementia would be denied statins). Most recently, new data from the Canadian Study of Health and Aging have produced a mixed result. While methodological considerations are clearly important in understanding why the reports are so variable, there might also be merit in differentiating between statins, based on their presumed – and variable – mechanisms of action in dementia prevention, before concluding that the initial reports are entirely artefactual. Still, the first reports appear to have overestimated the extent of protection, so that unless there are important effects achievable with specific statins, a more than a modest role for statins in preventing AD seems unlikely.” The second abstract is taken from reference [28], on the “alternative hypothesis” that amyloid-beta is protective rather than detrimental to Alzheimer’s, i.e., that it is a “protective response to neuronal insult:”
Abstract, “Amyloid-beta in Alzheimer disease: the null versus the alternate hypotheses:”
“For nearly 20 years, the primary focus for researchers studying Alzheimer disease has been centered on amyloid-beta, such that the amyloid cascade hypothesis has become the “null hypothesis.” Indeed, amyloid-beta is, by the current definition of the disease, an obligate player in pathophysiology, is toxic to neurons in vitro, and, perhaps most compelling, is increased by all of the human genetic influences on the disease. Therefore, targeting amyloid-beta is the focus of considerable basic and therapeutic interest. However, an increasingly vocal group of investigators are arriving at an “alternate hypothesis” stating that amyloid-beta, while certainly involved in the disease, is not an initiating event but rather is secondary to other pathogenic events. Furthermore and perhaps most contrary to current thinking, the alternate hypothesis proposes that the role of amyloid-beta is not as a harbinger of death but rather a protective response to neuronal insult. To determine which hypothesis relates best to Alzheimer disease requires a broader view of disease pathogenesis and is discussed herein.”
Contact: seneff@csail.mit.edu
References
[1] H. Akiyama, S. Barger, S. Barnum, B. Bradt, J.Bauer, G.M. Cole, N.R. Cooper, P. Eikelenboom, M. Emmerling, B.L. Fiebich, C.E. Finch, S. Frautschy, W.S. Griffin, H. Hampel, M. Hull, G. Landreth, L. Lue, R. Mrak, I.R. Mackenzie, P.L. McGeer, M.K. O’Banion, J. Pachter, G. Pasinetti, C. Plata-Salaman, J. Rogers, R.Rydel, Y. Shen, W. Streit, R. Strohmeyer, I. Tooyoma, F.L. Van Muiswinkel, R. Veerhuis, D. Walker, S. Webster, B. Wegrzyniak, G. Wenk, and T. Wyss-Coray, “Inflammation and Alzheimer’s disease.” Neurobiol Aging (2000) May-Jun;21(3):383-421,
[2] Alzheimer’s Association, “Alzheimer’s Disease Facts and Figures,” Alzheimer’s and Dementia (2009) Vol. 5, Issue 3.
[3] K.J. Anstey, D.M. Lipnicki and L.F. Low, “Cholesterol as a risk factor for dementia and cognitive decline: a systematic review of prospective studies with meta-analysis.” Am J Geriatr Psychiatry (2008) May, Vol. 16, No. 5, pp. 343-54.
[4] G. Arendash, A. Cox, T. Mori, J. Cracchiolo, K. Hensley, J. Roberts 2nd, “Oxygen treatment triggers cognitive impairment in Alzheimer’s transgenic mice,” Neuroreport. (2009) Jun 18.
[5] B.J. Balin, C.S. Little, C.J. Hammond, D.M. Appelt, J.A. Whittum-Hudson, H.C. Gerard, A.P. Hudson, “Chlamydophila pneumoniae and the etiology of late-onset Alzheimer’s disease.” J. Alz. Dis. (2008) Vol. 13, pp. 371-380.
[6] G. Bartzokis, MD; P.H. Lu, Psy, D.H. Geschwind, MD, N.Edwards, MA, J. Mintz, PhD, and J.L. Cummings, MD, “Apolipoprotein E Genotype and Age-Related Myelin Breakdown in Healthy Individuals: Implications for Cognitive Decline and Dementia,” Arch Gen Psychiatry (2006) Vol. 63, pp. 63-72.
[7] N. Bernoud, L. Fenart, C. Bénistant, J. F. Pageaux, M. P. Dehouck, P. Molière, M. Lagarde, R. Cecchelli,d, and J. Lecerf, “Astrocytes are mainly responsible for the polyunsaturated fatty acid enrichment in blood-brain barrier endothelial cells in vitro” Journal of Lipid Research (1998) Sept., Vol. 39, pp. 1816-1824.
[8] M. S. Brown and J. L. Goldstein, “A Receptor-Mediated Pathway for Cholesterol Homeostasis,” Nobel Lecture, December 9, 1985.
[9] N. Cartier, C. Sevin, A. Benraiss, P. DeDeyn, D. Bonnin, M-T Vanier, M. Philippe, V. Gieselmann and P. Aubourg, “AAV5-Mediated Delivery of Human Aryl Sulfatase A (hARSA) Prevents Sufatide Storage and Neuropathological Phenotype in Metachromatic Leukodystrophy (MLD) Mice,” Molecular Therapy (2005) 11, S166-S167; doi: 10.1016/j.ymthe.2005.06.431
[10] J. Chavarro, W.C. Willett, and P.J. Skerrett, The Fertility Diet, (2008) McGraw Hill.
[11] L.C. Costantini, L.J. Barr, J.L. Vogel and S.T. Henderson, “Hypometabolism as a therapeutic target in Alzheimer’s disease” BMC Neurosci (2008) Vol. 9, Suppl. 2, S16. doi: 10.1186/1471-2202-9-S2-S16.
[12] V. Demarin, S.S. Podobnik, D. Storga-Tomic and G. Kay, “Treatment of Alzheimer’s disease with stabilized oral nicotinamide adenine dinucleotide: A randomized, double-blind study” Drugs Exp Clin Res. (2004) Vol. 30, No. 1, pp. 27-33.
[13] R.B. DeMattos, R.P. Brendza, J.E. Heuser, M.Kierson, J.R. Cirrito, J. Fryer, P.M. Sullivan, A.M. Fagan, X. Han and D.M. Holtzman, “Purification and characterization of astrocyte-secreted apolipoprotein E and J-containing lipoproteins from wild-type and human apoE transgenic mice,” Neurochem Int. (2001) Nov-Dec;39(5-6):415-25. doi:10.1016/S0197-0186(01)00049-3.
[14] M. Dezfulian, M.A. ShokrgozarA, S. Sardari, K. Parivar and G. Javadi, “Can phages cause Alzheimer’s disease?” Med Hypotheses (2008) Nov;71(5):651-6.
[15] B.A. Golomb, M.D., Ph.D., “Statin Adverse Effects: Implications for the Elderly,” Geriatric Times (2004) May/June, Vol. V, Issue 3
[16] W.R. Grant, Ph.D., “Does Vitamin D Reduce the Risk of Dementia?” Journal of Alzheimer’s Disease (2009) May, Vol. 17, No. 1., pp. 151-9.
[17] Dr. Duane Graveline, Lipitor: Thief of Memory, Statin Drugs and the Misguided War on Cholesterol, (2004) http://www.buybooksontheweb.com.
[18] X. Han, “Potential mechanisms contributing to sulfatide depletion at the earliest clinically recognizable stage of Alzheimer’s disease: a tale of shotgun lipidomics,” J Neurochem (2007) November, Vol. 103, Suppl. 1. pp. 171-179. doi: 10.1111/j.1471-4159.2007.04708.x.
[19] X. Han, H. Cheng, J.D. Fryer, A.M. Fagan and D.M. Holtzman, “Novel Role for Apolipoprotein E in the Central Nervous System: Modulation of Sulfatide Content” Journal of Biological Chemistry, March 7, 2003, Vol. 278, pp. 8043-8051, DOI 10.1074/jbc.M212340200.
[20] K. Heininger, “A unifying hypothesis of Alzheimer’s disease. IV. Causation and sequence of events,” Rev Neurosci. (2000) Vol. 11, Spec No, pp.213-328.
[21] S.T. Henderson, “Ketone Bodies as a Therapeutic for Alzheimer’s Disease,” NeuroTherapeutics,, (2008) Jul;5(3):470-80, doi:10.1016/j.nurt.2008.05.004
[22] S. Holmberg, A. Thelin and E.-L. StiernstrNvm, “Food Choices and Coronary Heart Disease: A Population Based Cohort Study of Rural Swedish Men with 12 Years of Follow-up,” Int. J. Environ. Res. Public Health (2009) Vol. 6, pp. 2626-2638;
[23] K. Honjo, R. van Reekum, and N.P. Verhoeff, “Alzheimer’s disease and infection: do infectious agents contribute to progression of Alzheimer’s disease?” Alzheimers Dement. (2009) Jul;5(4):348-60.
[24] S.M. Innis and R.A. Dyer, “Brain astrocyte synthesis of docosahexaenoic acid from n-3 fatty acids is limited at the elongation of docosapentaenoic acid,” (2002) Sept. Journal of Lipid Research, Vol. 43, pp. 1529-1536.
[25] L. Jeng, A.V. Yamshchikov, S.E. Judd, H.M. Blumberg, G.S. Martin, T.R. Ziegler and V. Tangpricha, “Alterations in Vitamin D Status and Anti-microbial Peptide Levels in Patients in the Intensive Care Unit with Sepsis,” Journal of translational Medicine,” (2009) Vol. 7, No. 28.
[26] J. Kountouras, M. Boziki, E. Gavalas, C. Zavos, G. Deretzi, N. Grigoriadis, M. Tsolaki, D. Chatzopoulos, P. Katsinelos, D. Tzilves, A. Zabouri, I. Michailidou, “Increased cerebrospinal fluid Helicobacter pylori antibody in Alzheimer’s disease,” Int J Neurosci. (2009) 119(6):765-77.
[27] J. Kountouras, M. Boziki, E. Gavalas, C. Zavos, N. Grigoriadis, G. Deretzi, D. Tzilves, P. Katsinelos, M. Tsolaki, D. Chatzopoulos, and I. Venizelos, “Eradication of Helicobacter pylori may be beneficial in the management of Alzheimer’s disease,” J Neurol. (2009) May;256(5):758-67. Epub 2009 Feb 25.
[28] H.G. Lee, X. Zhu, R.J. Castellani, A. Nunomura, G. Perry, and M.A. Smith, “Amyloid-beta in Alzheimer disease: the null versus the alternate hypotheses,” J Pharmacol Exp Ther. (2007) June, Vol. 321 No. 3, pp. 823-9. doi:10.3390/ijerph6102626.
[29] J. Marcus, S. Honigbaum, S. Shroff, K. Honke, J. Rosenbluth and J.L. Dupree, “Sulfatide is essential for the maintenance of CNS myelin and axon structure,” Glia (2006), Vol. 53, pp. 372-381.
[30] R.T. Matthews, L. Yang, S. Browne, M. Baik and M.F. Beal, “Coenzyme Q10 administration increases brain mitochondrial concentrations and exerts neuroprotective effects,” Proc Natl Acad Sci U S A. (1998) Jul 21, Vol. 95, No. 15, pp.8892-7.
[31] D. Lutjohann and K. von Bergmann, “24S-hydroxycholesterol: a marker of brain cholesterol metabolism”Pharmacopsychiatry (2003) January 10, Vol. 36 Suppl 2, pp. S102-6, DOI: 10.1055/s-2003-43053.
[32] J. C. McCann and B.N. Ames, “Is there convincing biological or behavioral evidence linking vitamin D deficiency to brain dysfunction?”, (2008) FASEB J. Vol. 22, pp. 982-1001. doi: 10.1096/fj.07-9326rev.
[33] Larry McCleary, M.D., The Brain Trust Program (2007) September, The Penguin Group, New York, New York.
[34] B. McGuinness et al., “Statins for the prevention of dementia,” Cochrane Database of Systematic Reviews,(2009) No. 2.
[35] M.M. Mielke, P.P. Zandi, M. Sjogren, et al. “High total cholesterol levels in late life associated with a reduced risk of dementia,” Neurology (2005) Vol. 64, pp. 1689-1695.
[36] S.A. Moore, “Polyunsaturated Fatty Acid Synthesis and Release by Brain-Derived Cells in Vitro,” Journal of Molecular Neuroscience (2001), Vol. 16, pp. 195ff.
[37] D. Mozaffarian, E.B. Rimm, D.M. Herrington, “Dietary fats, carbohydrate, and progression of coronary atherosclerosis in postmenopausal women,” Am J Clin Nutr (2004) Vol. 80, pp. 1175-84.
[38] M. Mulder, R. Ravid, D.F. Swaab, E.R. de Kloet, E.D. Haasdijk, J. Julk, J.J. van der Boom and L.M. Havekes, “Reduced levels of cholesterol, phospholipids, and fatty acids in cerebrospinal fluid of Alzheimer disease patients are not related to apolipoprotein E4,” Alzheimer Dis Assoc Disord. (1998) Sep, Vol. 12, No. 3, pp. 198-203.
[39] I.L. Notkola, R. Sulkava, J. Pekkanen, T. Erkinjuntti, C. Ehnholm, P. Kivinen, J. Tuomilehto, and A. Nissinen, “Serum total cholesterol, apolipoprotein E epsilon 4 allele, and Alzheimer’s disease,” Neuroepidemiology (1998) Vol. 17, No. 1, pp. 14-20.
[40] F.W. Pfrieger, “Outsourcing in the brain: Do neurons depend on cholesterol delivery by astrocytes?”, BioEssays(2003) Vol. 25 Issue 1, pp.72-78.
[41] A. Phivilay, C. Julien, C. Tremblay, L. Berthiaume, P. Julien, Y. Giguère and F. Calon, “High dietary consumption of trans fatty acids decreases brain docosahexaenoic acid but does not alter amyloid-beta and tau pathologies in the 3xTg-AD model of Alzheimer’s disease.” Neuroscience (2009) Mar 3, Vol. 159, No. 1, pp. 296-307. Epub 2008 Dec 14.
[42] M.A. Reger, S. T. Henderson, C. Hale, B. Cholerton, L.D. Baker, G.S. Watson, K. Hyde, D. Chapman and S. Craft, “Effects of Beta-hydroxybutyrate on cognition in memory-impaired adults,” Neurobiology of Aging (2004) Vol. 25, No. 3, March, pp. 311-314,
[43] R. Ringseis, C. Dathe, A. Muschick, C. Brandsch and K. Eder, “Nutrient Physiology, Metabolism, and Nutrient-Nutrient Interactions Oxidized Fat Reduces Milk Triacylglycerol Concentrations by Inhibiting Gene Expression of Lipoprotein Lipase and Fatty Acid Transporters in the Mammary Gland of Rats,” American Society for Nutrition J. Nutr. (2007) Sept., Vol. 137, pp. 2056-2061.
[44] K. Rockwood, “Epidemiological and clinical trials evidence about a preventive role for statins in Alzheimer’s disease.” Acta Neurol Scand Suppl. (2006) Vol. 185, pp. 71-7.
[45] G. Saher, B. Brugger, C. Lappe-Siefke, W. Mobius, R. Tozawa, M.C. Wehr, F. Wieland, S. Ishibashi, and K.A. Nave, “High cholesterol level is essential for myelin membrane growth.” Nat Neurosci (2005) Apr, Vol. 8, No. 4, pp. 468-75. Epub 2005 Mar 27.
[46] A. Solomon, M. Kivipelto, B. Wolozin, J. Zhou, and R.A. Whitmer, “Midlife Serum Cholesterol and Increased Risk of Alzheimer’s and Vascular Dementia Three Decades Later,” Dementia and Geriatric Cognitive Disorders (2009) Vol. 28, pp. 75-80, DOI: 10:1159/000231980.
[47] M. Simons, MD, P. Keller, PhD, J. Dichgans, MD and J.B. Schulz, MD, “Cholesterol and Alzheimer’s disease: Is there a link?” Neurology (2001) Vol. 57, pp. 1089-1093.
[48] L.L. Smith, “Another cholesterol hypothesis: cholesterol as antioxidant,” Free Radic Biol Med. (1991) Vol. 11, No. 1, pp. 47-61.
[49] E. Steen, B.M. Terry, E.J. Rivera, J.L. Cannon, T.R. Neely, R. Tavares, X.J. Xu, J.R. Wands, and S.M. de la Monte “Impaired insulin and insulin-like growth factor expression and signaling mechanisms in Alzheimer’s disease – is this type 3 diabetes?” Journal of Alzheiner’s Disease (2005) Vol. 7, Number 1, pp. 63-80.
[50] J. Tong, P.P. Borbat, J.H. Freed and Y-K Shin, “A scissors mechanism for stimulation of SNARE-mediated lipid mixing by cholesterol,” PNAS (2009) March 31 Vol. 106, No. 13, pp. 5141-5146.
[51] M-C Vohl, T. A.-M. Neville, R. Kumarathasan, S. Braschi, and D.L. Sparks, “A Novel Lecithin-Cholesterol Acyltransferase Antioxidant Activity Prevents the Formation of Oxidized Lipids during Lipoprotein Oxidation,”Biochemistry (1999) Vol. 38 No. 19, pp. 5976-5981. DOI: 10.1021/bi982258w.
[52] M. Waldman, MD,, 9th International Conference on Alzheimer’s and Parkinson’s Diseases (2009) Abstract 90, Presented March 12-13.
[53] R. West, M.A., M. Schnaider Beeri, Ph.D., J. Schmeidler, Ph.D., C. M. Hannigan, B.S., G. Angelo, M.S., H.T. Grossman, M.D., C. Rosendorff, M.D., Ph.D., and J.M. Silverman, Ph.D., “Better memory functioning associated with higher total and LDL cholesterol levels in very elderly subjects without the APOE4 allele,” Am J Geriatr Psychiatry(2008) September; Vol. 16, No. 9, pp. 781-785. doi: 10.1097/JGP.0b013e3181812790.
[54] A.W.E. Weverling-Rijnsburger, G.J. Blauw, A.M. Lagaay, D.L. Knook, A.E. Meinders, and R.G.J. Westendorp, “Total cholesterol and risk of mortality in the oldest old,” The Lancet, (1997) Vol. 350, No. 9085, pp. 1119-1123,
[55] R.F. Wilson, J.F. Barletta and J.G. Tyburski, “Hypocholesterolemia in Sepsis and Critically Ill or Injured Patients”Critical Care (2003), Vol. 7, pp. 413-414.
[56] S.-C. Zhang and S. Fedoroff, “Neuron-microglia Interactions in Vitro,” Acta Neuropathol (1996) Vol. 91, pp. 385-395.
September 20, 2021 Posted by aletho | Book Review, Science and Pseudo-Science, Timeless or most popular | alzheimer's, Cholesterol, Statins, Vitamin D | Leave a comment
Is the cholesterol hypothesis dead?
Sebastian Rushworth, M.D. | September 8, 2020
Is there any life left in the cholesterol hypothesis (a.k.a. the lipid hypothesis)? Is there anything left for serious scientists to cling to or is time for its mouldering corpse to end up on the trash heap of medical history, alongside lobotomy, bloodletting and the theory of the four humors? I was asked this question by a reader of this blog recently, and as it happens, a systematic review was recently published in Evidence Based Medicine (my favorite medical journal, mainly because it is edited by the brilliant Dr. Carl Heneghan) that definitively answers this question, so I thought it would be interesting to go through what the evidence says together.
As many readers will be aware, the cholesterol hypothesis is the idea that cardiovascular disease is caused by high levels of cholesterol in the blood stream. The hypothesis harks back to the early part of the twentieth century, when a Russian researcher named Nikolai Anitschkow fed a cholesterol rich diet to rabbits and found that they developed atherosclerosis (hardening of the arteries, the process which in the long run leads to cardiovascular disease). Of course, rabbits and humans are very different species, with very different dietary preferences. Rabbits, being herbivores, normally have very little cholesterol in their diets, while humans, being omnivores, generally consume quite a bit of cholesterol. Regardless, the data was suggestive, and led to the hypothesis being formulated.
In the 1940’s and 1950’s an American researcher named Ancel Keys carried out a number of studies which supposedly showed a correlation between cholesterol intake and heart disease in humans. The most famous of these was the “Seven Countries Study”, which was an observational study carried out in, as the name implies, seven different countries, and which found that people in countries with a high intake of saturated fat had high blood levels of cholesterol, and were much more likely to develop heart disease than people in countries with a low intake of saturated fat. This lead to the hypothesis that saturated fat intake leads to high blood cholesterol levels which leads to atherosclerosis which leads to cardiovascular disease and premature death.
As we’ve discussed before, observational studies cannot draw any conclusions about causation, they can only show correlation. And there is also a question why these seven specific countries were chosen (the reader will be aware that there are in fact closer to two hundred countries) – they certainly weren’t chosen at random. If the populations in a study aren’t chosen at random, that creates a significant risk of cherry picking of data (and makes it impossible for the researchers carrying out a study to refute that accusation).
In spite of these limitations, the cholesterol hypothesis became heavily hyped, leading to official dietary recommendations around the world, which are still very much unchanged, that recommend low intakes of saturated fat and cholesterol, and of foods rich in these substances, such as red meat.
The hypothesis also resulted in pharmaceutical companies investing huge sums in research to find a drug that would lower cholesterol levels in the blood. A number of drugs were discovered, but unfortunately, although they could lower cholesterol levels, none of them seemed to have any effect on mortality. People were dying at the same rate even with these drugs, sometimes even at higher rates. That was the first hit against the cholesterol hypothesis.
Then came statins, and everything changed. Statins are molecules that in nature are produced by certain types of fungi. Among other biological functions that aren’t completely understood, they inhibit an enzyme called HMG-CoA-reductase. This enzyme is central to the body’s ability to produce cholesterol. When it is blocked, cells are unable to produce their own cholesterol and have to find it from elsewhere. This causes them to express receptors on their surfaces that allow them to suck up cholesterol from the blood stream. This effect is most noticeable in the liver, since the liver is the body’s main cholesterol factory, and is the organ primarily responsible for recycling the molecules that transport cholesterol in the blood stream (cholesterol is a vital part of cell membranes so all cells in the body have the capacity to produce their own cholesterol). Since cholesterol is hoovered up from the blood stream, the cholesterol level in the blood drops. Yay!
The reason I say everything changed with statins is that they actually seemed to work. For the first time a drug had been discovered that lowered cholesterol and that also seemed to decrease mortality. Ancel Keys seemed to have been vindicated. Anyone suggesting that the cholesterol hypothesis was dead in the water was derided as a nut.
Now, as time has gone by, the cholesterol hypothesis has actually grown more complex, which is why doctors don’t really talk about cholesterol so much any more. Instead they talk about LDL, which stands for Low Density Lipoprotein. LDL is a transport molecule that is used to transport cholesterol in the blood stream (cholesterol is a lipid and as such is not soluble in blood, so it needs to be transported in a special transport molecule). This is important, because in the updated version of the hypothesis, it’s not the cholesterol itself that’s bad, it’s the LDL. Basically, the idea is that LDL that’s moving around in the body can become oxidized. Oxidized LDL can get stuck in artery walls, and start an inflammatory process that leads to atherosclerosis. So what statins actually do is cause the liver to hoover up LDL molecules from the blood stream, which prevents them from becoming oxidized in the tissues and causing atherosclerosis.
Now, unfortunately for the pharmaceutical companies, there are patent laws, which mean that after a couple of decades, their drugs go off-patent and they are no longer able to make big profits. Which is why they have developed newer types of cholesterol lowering drugs. There is ezetimibe, which works by inhibiting the uptake of cholesterol from the intestine. Most recently there are the PCSK9-inhibitors, which increase the liver’s uptake of LDL by preventing it from recycling the LDL-receptors on its surface, which results in more receptors on the surface and therefore a higher uptake of LDL from the blood stream.
Since there has been such widespread agreement that the cholesterol hypothesis is true, and that drugs that lower LDL also lower heart disease, cardiologists’ organizations around the world have set targets for LDL levels in the blood stream. For example, the American Heart Association and the American College of Cardiologists have set a target LDL reduction of 50% for people at high risk of cardiovascular disease, and 30% for people at moderate risk. Basically, people at high or moderate risk should be started on one cholesterol lowering drug, and if this drug doesn’t have a big enough effect on their LDL levels, then a second drug should be added. If enough effect still isn’t seen, then a third drug can be added, and so on until the target is reached.
Clearly, if the cholesterol hypothesis is true, then the amount of benefit seen from lowering LDL should stand in direct proportion to the amount by which LDL is lowered, right? Anything else would be illogical.
This brings us nicely to the recent systematic review in Evidence Based Medicine. The review looked at all randomized controlled trials involving either a statin, ezetimibe, or a PCSK-9 inhibitor, in which data was provided on both the level of LDL-reduction and mortality, and in which the treatment period was at least one year. The authors declared no conflicts of interest and received no outside funding in order to carry out the review.
In total, 35 trials were included in the review, with the smallest trial containing 249 participants, and the largest trial containing 27,564 participants. The total number of participants across all the trials was over 230,000. 29 of the 35 trials had over 1,000 participants. Basically, these were for the most part large, high quality studies. That should certainly be enough data to tell us definitively whether the cholesterol hypothesis is dead or alive.
The trials were sorted based on whether they were treating people with moderate risk of cardiovascular disease or people with high risk, and then further grouped based on whether the participants on average met the official American LDL targets (at least a 30% reduction in LDL for people with moderate risk, and at least a 50% reduction for people with high risk).
Here’s what they found:
Of the 13 trials that successfully met the LDL targets, only one was able to find a beneficial effect on mortality. Of the 22 trials that did not meet the LDL targets, four reported a mortality benefit. So, overall, only 5 out of 35 trials were able to find a mortality benefit, and four of those that did find a benefit did not lower LDL to the target level.
Furthermore, some trials that saw significant LDL reductions (over 50%) were not able to show any effect on mortality, while other trials in which LDL only dropped by 11-15% did see a significant effect on mortality. Basically, less LDL-lowering actually seemed to be better in terms of mortality than more LDL-lowering.
So, what can we conclude?
Firstly, yes, the cholesterol hypothesis is dead, dead, dead. There is no correlation between effect on LDL and effect on mortality. Anyone who still chooses to cling to the cholesterol hypothesis in spite of this is consciously refusing to see what a vast amount of high quality scientific evidence is putting right in front of their eyes.
Secondly, as an interesting aside, only 5 out of 35 trials found a mortality benefit, which means that 30 out of 35 did not find any benefit. And yet somehow statins are one of the most widely prescribed drugs in the world. Personally, if I look at an entire evidence base consisting of 35 trials, with a total of 230,000 patients, and 30 of those trials, with 195,000 people, fail to find a mortality benefit, then that’s going to make me think the treatment doesn’t work. At least not if the point of the treatment is to make people live longer.
So what are the practical implications for you as a patient? As I mentioned in an earlier article, there is no point getting your cholesterol levels tested, because they tell you nothing about your risk of cardiovascular disease. If you are already on a cholesterol lowering drug, and intend to continue for whatever reason, there is no point doing annual check-ups of your cholesterol levels, because there is no correlation between how much the drug lowers those levels and your risk of future cardiovascular events. And there is certainly no point in trying to reach a “target” LDL level.
October 13, 2020 Posted by aletho | Science and Pseudo-Science, Timeless or most popular | Statins | Leave a comment
Financial Conflicts & the Retracted COVID Research
Lead author, paid by drug companies, gives the all-clear to products those companies sell. World’s leading medical journal fails transparency test.
By Donna Laframboise | Big Picture News | June 22, 2020
Mandeep Mehra is a professor at Harvard Medical School, and the medical director of a Boston hospital department. That city being a coronavirus hotspot, life hasn’t been normal there for some time.
He’s also the lead author of two COVID-19 research papers that were retracted shortly after being published in prestigious medical journals. Lancet boss Richard Horton calls the one published in his journal a “monumental fraud.”
The other, which has received less attention, appeared in the New England Journal of Medicine (NEJM). Titled Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19, it runs to seven pages and was retracted because its authors now admit the data on which it relies cannot be validated.
During this pandemic, physicians have been desperate for information to help guide their decisions. Eric Rubin, editor-in-chief of the NEJM, recently explained to the New York Times,
I’m an infectious disease doctor, I treat Covid-19 patients. I’ve been in the hospital recently treating patients, and we have no idea what to do. I’m the primary driver at the journal of saying, ‘We have to get data out there that people can use.’ [bold added]
Many hypotheses have been advanced. Many questions remain unanswered. For example, there’s uncertainty about whether some widely prescribed medications might be complicating the picture. Are people who take high blood pressure pills – ACE inhibitors and ARBs (angiotensin receptor blockers) – at higher risk? Should they switch to alternatives until the pandemic is over (see here, here, and here)?
Similarly, should people on cholesterol-lowering statins follow advice published in the British Medical Journal and stop taking these drugs if they develop a serious case of COVID-19? Statins are, after all, prescribed for preventative purposes, to help avert heart problems longer term.
Mehra’s paper claimed to have examined patient records from three continents and to have found no evidence that any of these drugs increase the death rate of those who had heart issues prior to the coronavirus. Indeed, it declares that “the use of ACE inhibitors, and the use of statins were associated with a better chance of survival” in women.
But even if this data was 100% reliable, there would still be two enormous problems with this research:
#1: The lead author has financial ties to companies that sell those drugs.
#2: Neither the authors nor the journal informed us of this salient fact up front, in a transparent manner.
The paper reports, on page 1, that the research was “Funded by the William Harvey Distinguished Chair in Advanced Cardiovascular Medicine at Brigham and Women’s Hospital.”
Mehra’s Harvard e-mail address also appears on page 1. Readers are told that’s where reprint requests should be addressed (reprints are frequently distributed to third party doctors by drug companies as marketing material, and can be a considerable source of revenue for medical journals).
At the very end of the paper, on page 7, in fine print, we’re reminded that the research was supported by the William Harvey Distinguished Chair. Only then are we advised that “Disclosure forms by the authors are available with the full text of this article at NEJM.org.”
One must go to the trouble of tracking down the online version of the paper, and downloading that separate 16-page PDF, to discover the lead author has a serious conflict of interest. There, on page 12, we read:
Dr. Mehra reports personal fees from Abbott, personal fees from Medtronic, personal fees from Janssen, personal fees from Mesoblast , personal fees from Baim Institute for Clinical Research, personal fees from Portola, personal fees from Bayer, personal fees from Triple Gene, personal fees from Leviticus, personal fees from NupulseCV, personal fees from FineHeart, other from Riovant, outside the submitted work;. [sic, bold added]
Abbott Laboratories sells statins and ACE inhibitors. The company is described as a “top key player,” a “major giant,” and a “leading player” in those global marketplaces.
Likewise, Bayer AG is a major global player in the ARB market.
So a lead author who has financial relationships with two companies that sell certain classes of drugs took the time, during a pandemic, to give those drugs an all-clear.
On it’s website, the New England Journal of Medicine calls itself “the world’s leading medical journal.” Why did it choose to bury this vital piece of information?
June 22, 2020 Posted by aletho | Corruption, Deception, Science and Pseudo-Science | Covid-19, New England Journal of Medicine, Statins | Leave a comment
Why the Low Fat Diet Makes You Fat (and Gives You Heart Disease, Cancer and Tooth Decay)
Book review by Dr Stuart Jeanne Bramhall | February 12, 2015
The Truth About Animal Fat: What the Research Shows
 The Big Fat Surprise: Why Butter, Meat and Cheese Belong in a Healthy Diet lays out the scientific case why our bodies are healthiest on a diet rich in saturated fat from animal products. Analyzing study after study, Nina Teicholz leaves no doubt that the number one cause of the global epidemic of obesity, diabetes and heart disease is the low fat high carbohydrate diet doctors have been pushing for fifty years.
The Big Fat Surprise: Why Butter, Meat and Cheese Belong in a Healthy Diet lays out the scientific case why our bodies are healthiest on a diet rich in saturated fat from animal products. Analyzing study after study, Nina Teicholz leaves no doubt that the number one cause of the global epidemic of obesity, diabetes and heart disease is the low fat high carbohydrate diet doctors have been pushing for fifty years.
Blaming the Victim
My initial reaction on learning how the low fat diet became official government policy was to feel ripped off and angry. For decades, the medical establishment has been blaming fat people for being obese, portraying them as weak willed and lacking in self control. It turns out the blame lay squarely with their doctors, the American Heart Association (AHA), the US Department of Agriculture (USDA), Congress and the food manufacturers who fund the AHA (Proctor and Gamble, Nabisco, General Foods, Heinz, Quaker Oats and Corn Products Refining Corporation) for foisting a diet on them that increases appetite and weight gain.
The low fat diet is based on a “theory” put forward in the 1950s that heart disease was caused by elevated cholesterol levels – and a few deeply flawed epidemiological studies. In other words, the low fat diet is a giant human experiment the medical profession conducted on the American public while attempting to prove that saturated animal fats cause heart disease. Fifty years of research would show the exact opposite: not only do low fat high carbohydrate diets increase the risk of cardiac death, but they’re also responsible for a myriad of other health problems, with obesity and diabetes being the most problematic.
The studies Teicholz cites also debunk the myth that animal fat increases the risk of breast and colon cancer.
Heart Attacks Rare Prior to 1900
Coronary artery disease and heart attacks were virtually unknown prior to 1900. When Ancel Keys, the father of the low fat diet, began his anti-fat crusade in the 1950s he claimed that industrialization and an improved standard of living had caused Americans to switch from a plant based diet to a diet that was higher in animal fats. This was total rubbish. Prior to 1900, Americans had always eaten a meat-based diet, in part because wild game was much more plentiful in North America than in Europe. Early cookbooks and diaries reveal that even poor families had meat or fish with every meal. Even slaves had 150 pounds of red meet a year, which contrasts unfavorably with 40-70 pounds of red meat in the current American diet.
What changed in the twentieth century was the introduction of cheaper vegetable fats into the American diet, starting with margarine and Crisco in the early 1900s.
Keys was also responsible for the theory, again without research evidence, that high cholesterol levels cause heart disease. This was also rubbish. Fifty years of research negates any link between either total cholesterol or LDL* cholesterol and heart disease. In study after study the only clear predictor of heart disease is reduced HDL. The same studies show that diets high in animal fats increase HDL, while those high in sugar, carbohydrates and vegetable oils reduce HDL.
Teicholz also discusses the role of statins (cholesterol lowering drugs) in this context. Statins do reduce coronary deaths, but this is due to their anti-inflammatory effect – not because of their effect on cholesterol.
Researchers Silenced and Sidelined
For decades, researchers whose findings linked low fat diets with higher rates of heart disease, cancer, stroke and tooth decay were systematically silenced and sidelined. As frequently happens with doctors and scientists who challenge the powerful health industry, their grants were cut off and, in some cases, their careers destroyed.
For fifty years, the medical establishment simply ignored the growing body of research linking the high sugar/carbohydrate component of the low fat diet to heart disease, as well as those linking vegetable oils to cancer. Vegetable oils oxidize when cooked, leading to the production of cancer causing compounds such as aldehyde, formaldehyde and 4-hydroxnonene (HCN). Unsurprisingly diets in which vegetable oils (other than olive oil) are the primary fat are linked with an increased incidence of cancer. Several studies overseas have found high levels of respiratory cancer in fast food workers exposed to superheated vegetable oils.
The Atkins Diet
The Big Fat Surprise includes a long section on the Atkins diet, a popular high fat/protein low carbohydrate weight reduction diet in the 70s and 80s. The use of a high fat low carbohydrate diet for weight loss dates back to 1862 and was heavily promoted by Sir William Osler in his 1892 textbook of medicine. According to Teicholz, recent controlled studies totally vindicate Dr Robert C Atkins, who was ridiculed as a dangerous quack during his lifetime. They also debunk claims that high levels of protein in the Atkins diet cause kidney damage. In addition to being perfectly safe, controlled studies show it to be extremely effective for weight loss and treating diabetes.
The USDA and AHA Quietly Reverse Themselves
As Teicholz points out in her conclusion, the nutrition researchers who blindly pursued their anti-fat campaign – and politicians and corporate funders who supported them – have done Americans an immense disservice by creating a virtual epidemic of obesity and diabetes.
A few years ago, the tide began to turn, largely due to the 29,000 subject Women’s Health Initiative launched in 1993. In 2013, the USDA and AHA quietly eliminated fat targets from the dietary recommendations. Because they made no real effort to publicize their change of heart, many doctors are still giving their patients the wrong dietary advice and hounding them about their cholesterol levels.
Dump the Skim Milk
The take home lesson from this book is that it’s virtually impossible to eat too many eggs or too much red meat, cheese, sausage and bacon. Americans (and their overseas English-speaking cousins) need to dump the skim milk and margarine down the sink because whole milk and butter are better for you. People need to go back to cooking with lard, bacon drippings and butter. Cooking with vegetable oils can give you cancer.
Anyone with a weight problem needs to totally eliminate sugar and carbohydrate (the Atkins diet recommends less than half a slice of bread a day).
And if your doctor hassles you about your cholesterol tell him or her to read this book.
*LDL (low density lipoprotein) is referred to as “bad cholesterol” due to its alleged link to heart disease. HDL (high density lipoprotein) or “good cholesterol” appears to provide some protective effect against heart disease.
March 21, 2015 Posted by aletho | Book Review, Science and Pseudo-Science, Timeless or most popular | American Heart Association, Cancer, Heart disease, Obesity, Saturated fat, Statins, Type 2 Diabetes, USDA, Vegetable oil | Leave a comment
Drug-Induced Dementia isn’t Alzheimer’s
By Dr. Gary G. Kohls | Global Research | February 26, 2015
“More than 50 conditions can cause or mimic the symptoms of dementia.” and “Alzheimer’s (can only be) distinguished from other dementias at autopsy.” – from a Harvard University Health Publication entitled What’s Causing Your Memory Loss? It Isn’t Necessarily Alzheimer’s
“Medications have now emerged as a major cause of mitochondrial damage, which may explain many adverse effects. All classes of psychotropic drugs have been documented to damage mitochondria, as have statin medications, analgesics such as acetaminophen, and many others.” – Neustadt and Pieczenik, authors of Medication-induced Mitochondrial Damage and Disease
“Establishing mitochondrial toxicity is not an FDA requirement for drug approval, so there is no real way of knowing which agents are truly toxic.” – Dr. Katherine Sims, Mass General Hospital –http://www.mitoaction.org
“It is difficult to get a man to understand something, when his salary depends upon his not understanding it!” – Upton Sinclair, anti-fascist, anti-imperialist American author who wrote in the early 20thcentury
“No vaccine manufacturer shall be liable… for damages arising from a vaccine-related injury or death.” – President Ronald Reagan, as he signed The National Childhood Vaccine Injury Act (NCVIA) of 1986, absolving drug companies from all medico-legal liability when children die or are disabled from vaccine injuries.
Over the past several decades there have been a number of well-financed campaigns, promoted by well-meaning laypersons, to raise public awareness to the plight of patients with dementia. Suspiciously, most of these campaigns that come from “patient support” groups lead the public to believe that every dementia patient has Alzheimer’s dementia (AD).
Not so curiously, it turns out that many – perhaps all – of these campaigns have been funded – usually secretly – by the very pharmaceutical companies that benefit economically by indirectly promoting the sale of so-called Alzheimer’s drugs. Such corporate-generated public relations “campaigns” are standard operating procedure for all of BigPharma drugs, especially its psychopharmaceutical drugs. BigPharma has found that the promotion and de-stigmatization of so-called “mental illnesses” (for which there are FDA-approved drugs) is a great tool for marketing their drugs.
Recently Alzheimer’s support groups all around the nation have been sponsoring the documentary about country singer Glen Campbell who has recently been diagnosed by his physicians with Alzheimer’s disease (of unknown etiology) despite the obvious fact that Campbell was infamous for his chronic heavy use of brain-damaging, dementia-inducing, addicting, and very neurotoxic drugs like cocaine and alcohol. And, just like so many other hard-living celebrities like the recently suicidal Robin Williams, Campbell was known to have received prescriptions of legal drugs from their prescribing boutique psychiatrists and physicians, just adding to the burden that their failing livers, brains and psyches had to endure.
Since it is known that Alzheimer’s disease can only be truly diagnosed by a microscopic examination of the cerebral cortex (at autopsy), we have to question the very alive Glen Campbell’s diagnosis. And we also have to question the veracity and motivations of the sponsoring patient support groups and their BigPharma sponsors.
Is the Alzheimer’s Epidemic Actually a Drug-Induced Dementia Epidemic?
Synchronous with the huge increases (over the past generation or so) in
1) the incidence of childhood and adult vaccinations,
2) the widespread use of psychotropic and statin (cholesterol-lowering) drug use, and
3) the increased ingestion of a variety of neurotoxic substances – including food additives, there has been a large parallel increase in the incidence of
a) chronic illnesses of childhood, including autistic spectrum disorders,
b) “mental illnesses of unknown origin”, and also
c) dementia, a multifactorial reality which, via clever marketing and the studied ignorance of what is scientifically known about the actual causes – and diagnosis – of dementia, which has been primarily – and mistakenly – referred to as Alzheimer’s disease (of unknown etiology).
It is important to ask and then demand an honest answer to the question “could there be a connection between America’s increasingly common over-prescribing of immunotoxic, neurotoxic, synthetic prescription drugs and vaccines and some of the neurodegenerative disorders that supposedly “have no known cause”?
Could the economically disabling American epidemic of autoimmune disorders, psychiatric disorders, autism spectrum disorders, etc (all supposedly of unknown origin) that have erupted over the past several decades be found to have recognizable root causes and therefore be treatable and, most importantly, preventable?
These are extremely important questions, especially in the case of the current dementia epidemic, because the so-called Alzheimer’s patient support groups seem to be totally unaware of the powerful evidence that prescription drugs known to damage brain cells (especially by poisoning their mitochondria) would be expected to cause a variety of neurological and psychological disorders because of the brain cell death that eventually happens when enough of the mitochondria (the microscopic hearts and lungs of every cell) have been wounded irretrievably or killed off. (See more info on drugs and mitochondria below.)
One of the big problems in America’s corporate-controlled culture, corporate-controlled media and corporate-controlled medical industries is that the giant pharmaceutical corporations, who are in the business of developing, marketing and selling known mitochondrial toxins (in the form of their drugs and vaccine ingredients) have a special interest in pretending that there is no known cause for the disorders that their synthetic chemicals are causing (or they use the unprovable “it’s probably genetic” subterfuge).
It should be a concern of everybody who knows a demented patient, that some AD patient support groups are known to be front groups for the pharmaceutical companies that profit from the marketing to patients and their doctors the disappointingly ineffective drugs for Alzheimer’s like Aricept, Exelon, Namenda, Hexalon, and Razadyne.
Prescription Drug-Induced – and Vaccine-Induced – Mitochondrial Disorders
Acquired mitochondrial disorders (as opposed to the relatively rare primary mitochondrial disorders like muscular dystrophy) that can be caused by commonly prescribed drugs are difficult to diagnose and are generally poorly understood by most practitioners. When I went to med school, nobody knew anything about what synthetic drugs or vaccines did to the mitochondria.
A lot of mitochondrial research, especially since the 1990s, has proven the connections between a variety of commonly prescribed medications and mitochondrial disorders. That evidence seems to have been cunningly covered-up by the for-profit pharma groups (who control medical education and much of the media) and various other powers-that-be because of the serious economic consequences if the information was allowed in the popular press. The stake-holders in the pharmaceutical and medical industries, most of whom profit mightily from the routine and increasing usage of neurotoxic drugs and vaccines, supposedly operating in the name of Hippocrates, would be very displeased if this information got out. I submit that BigPharma’s cover-up of the connections is totally unethical and, in the opinion of many other whistleblowers, criminal.
An Honest Patient Guide for Dementia Patients from Harvard!
So I was pleasantly surprised to find a reasonably honest guide for dementia patients on a Harvard University website.
(The entire guide can be accessed at http://www.helpguide.org/harvard/whats-causing-your-memory-loss.htm#top.)
The information at that website stated that there were over 50 conditions that could cause or mimic early dementia symptoms. I hadn’t been taught anything about that reality when I went to med school, and I doubt that many of my physician colleagues were either. And besides, what medical practitioner in our double-booked clinic environment, even if he or she was aware, has the time to thoroughly rule out the 50 conditions when confronted with a patient with memory loss?
I have often said to my patients and my seminar participants: “it takes only 2 minutes to write a prescription, but it takes 20 minutes to not write a prescription”. And in the current for-profit clinic culture, time is money and few physicians are given the “luxury” of spending adequate time with their patients. (In defense of the physicians that I know, they are not happy about that reality but don’t know what to do about it.)
It is so tempting to use the popularized, but rather squishy label of AD (of unknown etiology) rather than to educate ourselves about the possibility of drug- or vaccine-induced dementia. But what is so important is that many of the 50+ conditions are preventable or reversible, which will be therapeutic only if the conditions are identified before permanent brain damage occurs.
The Harvard guide actually said that “medications are common culprits in mental decline. With aging, the liver becomes less efficient at metabolizing drugs, and the kidneys eliminate them from the body more slowly. As a result, drugs tend to accumulate in the body. Elderly people in poor health and those taking several different medications are especially vulnerable.”
The guide continued with a list of the possible classes of prescription drugs that number in the hundreds:
“The list of drugs that can cause dementia-like symptoms is long. It includes antidepressants, antihistamines, anti-Parkinson drugs, anti-anxiety medications, cardiovascular drugs, anticonvulsants, corticosteroids, narcotics, sedatives.”
The Harvard guide went on to emphasize that Alzheimer’s can only be accurately diagnosed on a post-mortem examination. The guide states that “Alzheimer’s is distinguished from other dementias at autopsy by the presence of sticky beta-amyloid plaques outside brain cells (neurons) and fibrillary tangles within neurons (all indicative of cellular death). Although such lesions may be present in any aging brain, in people with Alzheimer’s these lesions tend to be more numerous and accumulate in areas of the brain involved in learning and memory.”
“The leading theory is that the damage to the brain results from inflammation and other biological changes that cause synaptic loss and malfunction, disrupting communication between brain cells. Eventually the brain cells die, causing tissue loss In imaging scans, brain shrinkage is usually first noticeable in the hippocampus, which plays a central role in memory function.”
But even the Harvard guide inexplicably failed to mention known mitochondrial toxins such as statin drugs, metformin, Depakote, general anesthetics, fluoroquinolone antibiotics, fluorinated psychotropic drugs, NutraSweet (every molecule of aspartame, when it reaches 86 degrees F, releases one molecule of the excitotoxin aspartic acid and one molecule of methanol [wood alcohol] which metabolizes into the known mitochondrial poison formaldehyde [embalming fluid]), pesticides (including the chlorinated artificial sweetener Splenda, which was initially developed as a pesticide) or the mercury (thimerosal), aluminum and formaldehyde which are common ingredients in vaccines. These are only some of the synthetic drugs that are capable of causing mitochondrial damage in brain cells – with memory loss, confusion and cognitive dysfunction, all early symptoms of dementia.
It is tragic, but all–too-common, for reversible and preventable drug-induced dementias (therefore of known cause and thus not Alzheimer’s) to be mis-diagnosed as Alzheimer’s disease “of unknown etiology” and to then be prescribed costly, essentially ineffective and potentially toxic drugs – whose mitochondrial toxicities have not been tested for.
(The pharmaceutical industry, it should be noted, is not required by the FDA to test its drugs for mitochondrial toxicity when it is doing its studies for marketing approval, again exhibiting the total disdain for the Precautionary Principle by both industry and the regulatory agencies such as the FDA, the CDC and WHO.)
There is much more in the basic neuroscience literature proving the connections, at least from authors who do not have conflicts of interest with BigPharma and BigMedicine. The authors of these articles have raised the questions and have published the proof that concerned families of patients and their physicians desperately need to know.
Don’t expect BigPharma to respond or to offer apologies or mea culpas. Do expect denials, dismissals, distractions, discrediting and then the delaying of real legitimate explorations of the real scientific evidence that exposes its subterfuge in the name of maintaining large profits for their stakeholders.
Here are the abstracts from just two of the many peer-reviewed articles from various science journals that support the thesis of this column.
Medication-induced mitochondrial damage and disease
Published in the Molecular Nutrition and Food Research journal ; 2008 Jul;52(7):780-8.
Authors: Neustadt, J, Pieczenik SR.
Abstract
Mitochondrial Dysfunction and Psychiatric Disorders
From: The Journal of Neurochemical Research 2009 Jun;34(6):1021-9.
Abstract
Mitochondrial oxidative phosphorylation is the major ATP-producing pathway, which supplies more than 95% of the total energy requirement in the cells. Damage to the mitochondrial electron transport chain has been suggested to be an important factor in the pathogenesis of a range of psychiatric disorders. Tissues with high energy demands, such as the brain, contain a large number of mitochondria, being therefore more susceptible to reduction of the aerobic metabolism. Mitochondrial dysfunction results from alterations in biochemical cascade and the damage to the mitochondrial electron transport chain has been suggested to be an important factor in the pathogenesis of a range of (so-called) neuropsychiatric disorders, such as (psychotropic drug-treated) bipolar disorder, depression and schizophrenia….Alterations of mitochondrial oxidative phosphorylation in (anti-psychotic drug-treated) schizophrenia have been reported in several brain regions and also in platelets. Abnormal mitochondrial morphology, size and density have all been reported in the brains of (anti-psychotic drug-treated) schizophrenic individuals. Considering that several studies link energy impairment to neuronal death, neurodegeneration and disease, this review article discusses energy impairment as a mechanism underlying the pathophysiology of some psychiatric disorders, like (psychotropic drug-treated) bipolar disorder, depression and schizophrenia.
Dr Kohls is a retired physician who practiced holistic mental health care for the last decade of his career, and took seriously the Hippocratic Oath that he swore when he received his medical degree. He is also a peace and justice advocate and writes a weekly column for the Reader Weekly, an alternative newsweekly published in Duluth, Minnesota, USA. The last three years of Dr Kohls’ columns are archived at http://duluthreader.com/articles/categories/200_Duty_to_Warn.
February 26, 2015 Posted by aletho | Deception, Science and Pseudo-Science | Acetaminophen, Aricept, CDC, Depakote, Exelon, FDA, Hexalon, Metformin, Namenda, NutraSweet, Razadyne, Splenda, Statins, WHO | Leave a comment
Featured Video
9/11 In Perspective
or go to
Aletho News Archives – Video-Images
From the Archives
Still No End in Sight of the Murder and Mayhem Wrought by the 9/11 Culprits
By Prof. Tony Hall | American Herald Tribune | July 17, 2016
The Kevin Barrett-Chomsky Dispute in Historical Perspective – Fourth part of the series titled “9/11 and the Zionist Question”
Back in 2006 all but a prescient few, such as Christopher Bollyn, perceived it as premature to try to identify and bring to justice the actual perpetrators of the 9/11 crimes. There was still some residue of confidence that responsible officials in government, law enforcement, media and the universities could and would respond in good faith to multiple revelations that great frauds had occurred in interpreting 9/11 for the public.
Accordingly, the main methodology of public intellectuals like Dr. Kevin Barrett or, for instance, Professors David Ray Griffin, Steven E. Jones, Peter Dale Scott, Graeme MacQueen, John McMurtry, Michael Keefer, Richard B. Lee, A.K. Dewdney, Nafeez Mossadeq Ahmed, and Michel Chossudovsky, was to marshal evidence demonstrating that the official narrative of 9/11 could not be true.
The marshaling of evidence was spurred on by observations coming from government insiders like Eckehardt Wertherbach, a former head of Germany’s intelligence service. In a meeting in Germany with Christopher Bollyn and Dr. Andreas von Bülow, Wertherbach pointed out that, “an attack of this magnitude and precision would have required years of planning. Such a sophisticated operation would require the fixed frame of a state intelligence organization, something not found in a loose group like the one led by the student Mohammed Atta in Hamburg.”
Andreas von Bülow was a German parliamentarian and Defense Ministry official. He confirmed this assessment in his book on the CIA and 9/11. In the text von Bülow remarked that the execution of the 9/11 plan “would have been unthinkable without backing from secret apparatuses of state and industry.” The author spoke of the “invented story of 19 Muslims working with Osama bin Laden in order the hide the truth” of the real perpetrators’ identity. … continue
Blog Roll
-
Join 2,403 other subscribers
Visits Since December 2009
- 7,384,842 hits
Looking for something?
Archives
Calendar
Categories
Aletho News Civil Liberties Corruption Deception Economics Environmentalism Ethnic Cleansing, Racism, Zionism Fake News False Flag Terrorism Full Spectrum Dominance Illegal Occupation Mainstream Media, Warmongering Malthusian Ideology, Phony Scarcity Militarism Progressive Hypocrite Russophobia Science and Pseudo-Science Solidarity and Activism Subjugation - Torture Supremacism, Social Darwinism Timeless or most popular Video War Crimes Wars for IsraelTags
9/11 Afghanistan Africa al-Qaeda Australia BBC Benjamin Netanyahu Brazil Canada CDC Central Intelligence Agency China CIA CNN Covid-19 COVID-19 Vaccine Donald Trump Egypt European Union Facebook FBI FDA France Gaza Germany Google Hamas Hebron Hezbollah Hillary Clinton Human rights Hungary India Iran Iraq ISIS Israel Israeli settlement Japan Jerusalem Joe Biden Korea Latin America Lebanon Libya Middle East National Security Agency NATO New York Times North Korea NSA Obama Pakistan Palestine Poland Qatar Russia Sanctions against Iran Saudi Arabia Syria The Guardian Turkey Twitter UAE UK Ukraine United Nations United States USA Venezuela Washington Post West Bank WHO Yemen Zionism
 Aletho News
Aletho News- Kaja Kallas: an uncomfortable figure useful to the EU’s Russophobic purposes
- German state blacklists right-wing party for first time
- Romania’s stolen elections were only the start: Inside the EU’s war on democracy
- Hawaii bills would allow gov’t to quarantine people, enter property without permission, seize firearms, and suspend laws
- Epstein files may contain ‘crimes against humanity’ – UN
- UK Government Plans to Use Delegated Powers to Undermine Encryption and Expand Online Surveillance
- Epstein Files Expose Israeli Occupation of America
- The Mandelson Molecule: Exposing the Architecture of Cross-Border Political Suppression
- The U.S. Sanctions Cuban Journalist For Reporting On The U.S. Blockade
- Israeli firms transform cars into intelligence devices: Reports
 If Americans Knew
If Americans Knew- Why won’t Trump’s “Board of Peace” bring peace? – Not a ceasefire Day 131
- Help end the injustice against Shadi
- Israel’s Favorite American President
- Israel’s “Yellow Line” Is a Death Trap for Palestinians. We Drove Into It.
- Why Israel’s expanding occupation in Syria presents a critical legal test
- Gaza is not a natural disaster. It is the victim of genocide enabled by global inaction
- Netanyahu’s plan to “end” US aid to Israel is to give even more money under a different name
- Israel ceased firing on Gaza for just 15 days of the “ceasefire” – Not a ceasefire Day 130
- In Gaza, “rats run over our faces” – Not a ceasefire Day 129
- Israel-backed border guards, GHF-linked aid – Not a ceasefire Day 128
 No Tricks Zone
No Tricks Zone- Coal Power Back In Trend As Globe Tries To Keep Pace With Growing Demand For Power
- New Study: A 4°C Warmer Beaufort Sea Had ‘No Sea Ice’ 11,700 – 8200 Years Ago
- Unfudging The Data: Dutch Meteorological Institute Reinstates Early 20th Centruy Heat Waves It Had Erased Earlier
- German Gas Crisis…Chancellor Merz Allegedly Bans Gas Debate Ahead of Elections!
- Pollen Reconstructions Show The Last Glacial’s Warming Events Were Global, 10x Greater Than Modern
- Germany’s Natural Gas Storage Level Dwindles To Just 28%… Increasingly Critical
- New Study Rebuts The Assumption That Anthropogenic CO2 Molecules Have ‘Special’ Properties
- Climate Scientist Who Predicted End Of “Heavy Frost And Snow” Now Refuses Media Inquiries
- Polar Bear Numbers Rising And Health Improving In Areas With The Most Rapid Sea Ice Decline
- One Reason Only For Germany’s Heating Gas Crisis: Its Hardcore-Dumbass Energy Policy
Contact:
atheonews (at) gmail.com
Disclaimer
This site is provided as a research and reference tool. Although we make every reasonable effort to ensure that the information and data provided at this site are useful, accurate, and current, we cannot guarantee that the information and data provided here will be error-free. By using this site, you assume all responsibility for and risk arising from your use of and reliance upon the contents of this site.
This site and the information available through it do not, and are not intended to constitute legal advice. Should you require legal advice, you should consult your own attorney.
Nothing within this site or linked to by this site constitutes investment advice or medical advice.
Materials accessible from or added to this site by third parties, such as comments posted, are strictly the responsibility of the third party who added such materials or made them accessible and we neither endorse nor undertake to control, monitor, edit or assume responsibility for any such third-party material.
The posting of stories, commentaries, reports, documents and links (embedded or otherwise) on this site does not in any way, shape or form, implied or otherwise, necessarily express or suggest endorsement or support of any of such posted material or parts therein.
The word “alleged” is deemed to occur before the word “fraud.” Since the rule of law still applies. To peasants, at least.
Fair Use
This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of environmental, political, human rights, economic, democracy, scientific, and social justice issues, etc. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes. For more info go to: http://www.law.cornell.edu/uscode/17/107.shtml. If you wish to use copyrighted material from this site for purposes of your own that go beyond ‘fair use’, you must obtain permission from the copyright owner.
DMCA Contact
This is information for anyone that wishes to challenge our “fair use” of copyrighted material.
If you are a legal copyright holder or a designated agent for such and you believe that content residing on or accessible through our website infringes a copyright and falls outside the boundaries of “Fair Use”, please send a notice of infringement by contacting atheonews@gmail.com.
We will respond and take necessary action immediately.
If notice is given of an alleged copyright violation we will act expeditiously to remove or disable access to the material(s) in question.
All 3rd party material posted on this website is copyright the respective owners / authors. Aletho News makes no claim of copyright on such material.

